Introduction
Access to health care in rural and remote Australia is a complex and challenging issue that remains unresolved despite continued efforts to improve the distribution of the medical workforce. Underlying this issue is the need to recruit and retain medical health professionals rurally. Despite this being the focus of a plethora of research, much of our understanding of the factors that contribute to attracting and maintaining a rural workforce comes from single-institution and cross-sectional studies focusing predominantly on placement-based medical education1-6. Although this work has contributed significantly, it is generally agreed that multi-institution and longitudinal studies are needed to determine the broader and longer term impacts of rural medical education on medical students’ future practice location7-9. A previous similar large-scale longitudinal investigation of graduate practice destination has been described for nursing and allied health graduates10. However, to the authors’ knowledge, this collaboration forms the first longitudinal, multi-university program of work investigating the impact of complete rural immersion during medical school on successive cohorts of medical students and graduates.
The Australian Government has invested in a number of education and training programs designed to influence rural health workforce distribution, such as the Rural Health Multidisciplinary Training (RHMT) program, which includes the requirement for at least 25% of Australian domestic medical students to undertake a minimum of 1 year of their clinical training in a rural area11. The specific target for each university may vary, with some RHMT-funded university programs able to achieve substantially higher than 25%. Independent evaluation of the RHMT program undertaken in 2020 recommended strengthening research networks via multi-site, multi-university and cross-jurisdictional partnerships and identified a number of factors from the literature that are associated with rural medical workforce conversion. These factors, both contextual (eg rural background) and place-based (duration and setting of clinical placement and availability of postgraduate training programs)12 have, to date, largely been associated with rural workforce conversion in the context of extended rural clinical school placement. Other notable factors that may influence workforce conversion include cost, travel, professional/social isolation, and impact of rural setting on life partners and families (employment and education/school choices). Although important, these factors have not, as yet, been thoroughly investigated in the context of complete rural immersion during medical education and do not identify what it is about the student experience (course content and structure) that impacts on their conversion rate.
For the most part, rural medical education has to date consisted of either short-term or extended rural clinical school placements (rural pipeline – existing) and just three entirely rural medical programs. The ‘pipeline’ to rural practice is a concept described in the literature as a pathway for the recruitment and retention of a rural health workforce13,14. Potential engagement points along the rural pipeline include (1) rural background and (2) rural medical education (rural curriculum + rural immersion), followed by (3) vocational medical training (eg GP, specialist, rural generalist) and (4) continuous professional development for rural health workers. With the expansion of rurally based medical programs, a new rural pipeline is emerging (rural pipeline – emerging) that will allow students to undertake the entirety of their medical degree in a rural area (Fig1). Numerous studies have shown that extended rural clinical school placement is effective and associated with subsequent rural practice3,4,6,15-17. Studies have also shown that the length of rural immersion has a positive impact on graduates’ future practice location1,3,5,16. O’Sullivan and colleagues, for example, demonstrated a concomitant increase in rural practice with increased length of rural immersion3. Evidence of an additive effect of rural background and rural medical education is also building1,3,5,6,18. However, one recent study has shown that ‘openness’ to rural practice may be more nuanced than the effect of rural background and rural immersion alone19. Bingham and colleagues postulate that connection to community during rural immersion may be particularly important for future rural practice. Limited evidence is available regarding the effect of complete rural immersion on medical students’ practice intentions and realisation. It is possible that, with complete rural immersion, students may form a deeper connection to community over time; however, this remains to be seen.
The Murray–Darling Medical Schools Network (MDMSN) is an Australian Government initiative that has established a network of rurally based medical programs in New South Wales and Victoria20. MDMSN rural clinical schools are located in the southern part of the Murray–Darling Basin, in regional centres or large rural towns, classified as MM2 or 3, using the Australian Government Modified Monash (MM) Model geographical classifications21. For the purposes of this article, the term ‘rurally based’ will be used to encompass medical programs based in both regional (MM 2) and rural (MM 3–7) areas. The MDMSN is part of the Stronger Rural Health Strategy and builds on the existing RHMT program to allow students to study medicine entirely in a rural area. The initiative is intended to give students a broad understanding of rural life, the health of rural communities, and the organisation and delivery of rural and remote health services, with the goal of encouraging more practitioners to consider a career in rural or remote medical practice.
The MDMSN initiative offers a unique opportunity to undertake multi-institution and longitudinal research into rurally based end-to-end medical training programs. The current literature lacks a comprehensive, nationwide analysis of these programs, which could lead to the use of inconsistent methodologies and a lack of comparable data. Recent systematic reviews have also called for a more consistent approach to study design and use of definitions for critical concepts such as rurality18,22. This research collaboration is well placed to address this gap by developing a comparable national cohort dataset and applying a consistent methodology. By doing so, we aim to better understand the characteristics of students who embark on longitudinal rural training, and how their experiences and perceptions inform their career decisions regarding place of practice. The findings of this research could have important implications, such as informing policy decisions and guiding strategies to recruit and retain healthcare professionals in underserved rural areas.
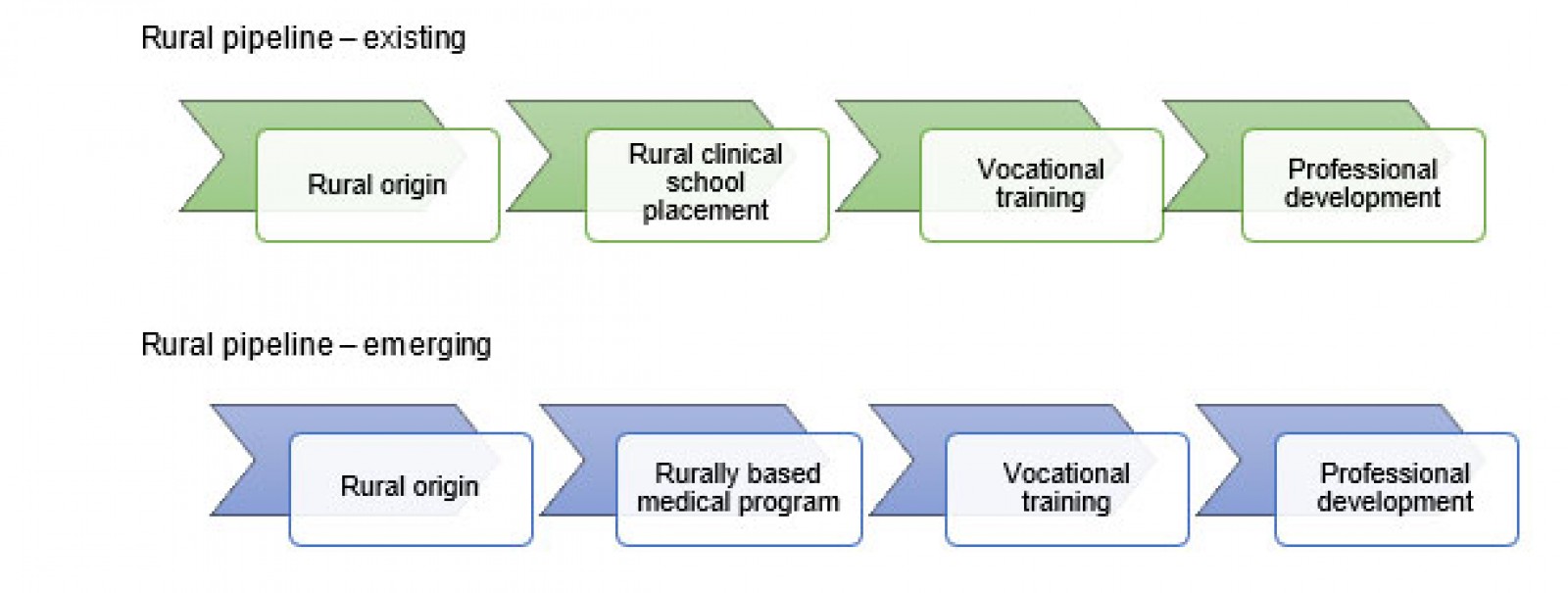 Figure 1: Australia’s rural medical education pipeline – existing and emerging.
Figure 1: Australia’s rural medical education pipeline – existing and emerging.
Methods
Context
The MDMSN research collaboration was established to ensure collaboration of partner universities from the outset of the MDMSN program and to harmonise prospective data collection. The collaboration was initiated by the University of Sydney (Dubbo – MM 3), who invited partner universities – the University of New South Wales (Wagga Wagga – MM 3), Charles Sturt University (Orange – MM 3) in partnership with Western Sydney University, Monash University (Churchill, Gippsland – MM 3, Bendigo – MM 2, Mildura – MM 3), and the University of Melbourne (Shepparton – MM 3) in partnership with La Trobe University – to discuss and develop a combined research initiative. Specifically, this is a longitudinal, multi-university program of work to explore the effect of rurally based medical school programs in the Murray–Darling region.
Aims and objectives
The aim of this research program is to develop a greater understanding of students undertaking rural medical education and ultimately add knowledge to address rural workforce maldistribution. Initial objectives were developed via expert consensus and a thorough study of the literature including existing national quantitative measures7,23 and the work undertaken by Sutton et al in the Nursing and Allied Graduate Outcomes Tracking (NAHGOT) study10:
- contextual factors of the new cohort of students embarking on rurally based medical education (objective 1)
- changes in practice intention over time (objective 2)
- place-based factors influencing intention (objective 3)
- rural practice realisation (objective 4).
Potential future objectives include:
- availability of rural internships, training places and professional development (objective 5)
- motivations for embarking on rurally based medical education (objective 6)
- changes in student professional identity over time (objective 7).
Participants
All students and graduates of the five participating medical programs will be invited to participate in this research. The inaugural cohort of medical students includes 147 potential participants from across the five participating medical programs (Table 1). Additional cohorts will be added annually, and each respective cohort will be tracked longitudinally following graduation.
Table 1: Characteristics of the cohorts of the five universities participating in the Murray–Darling Medical Schools Network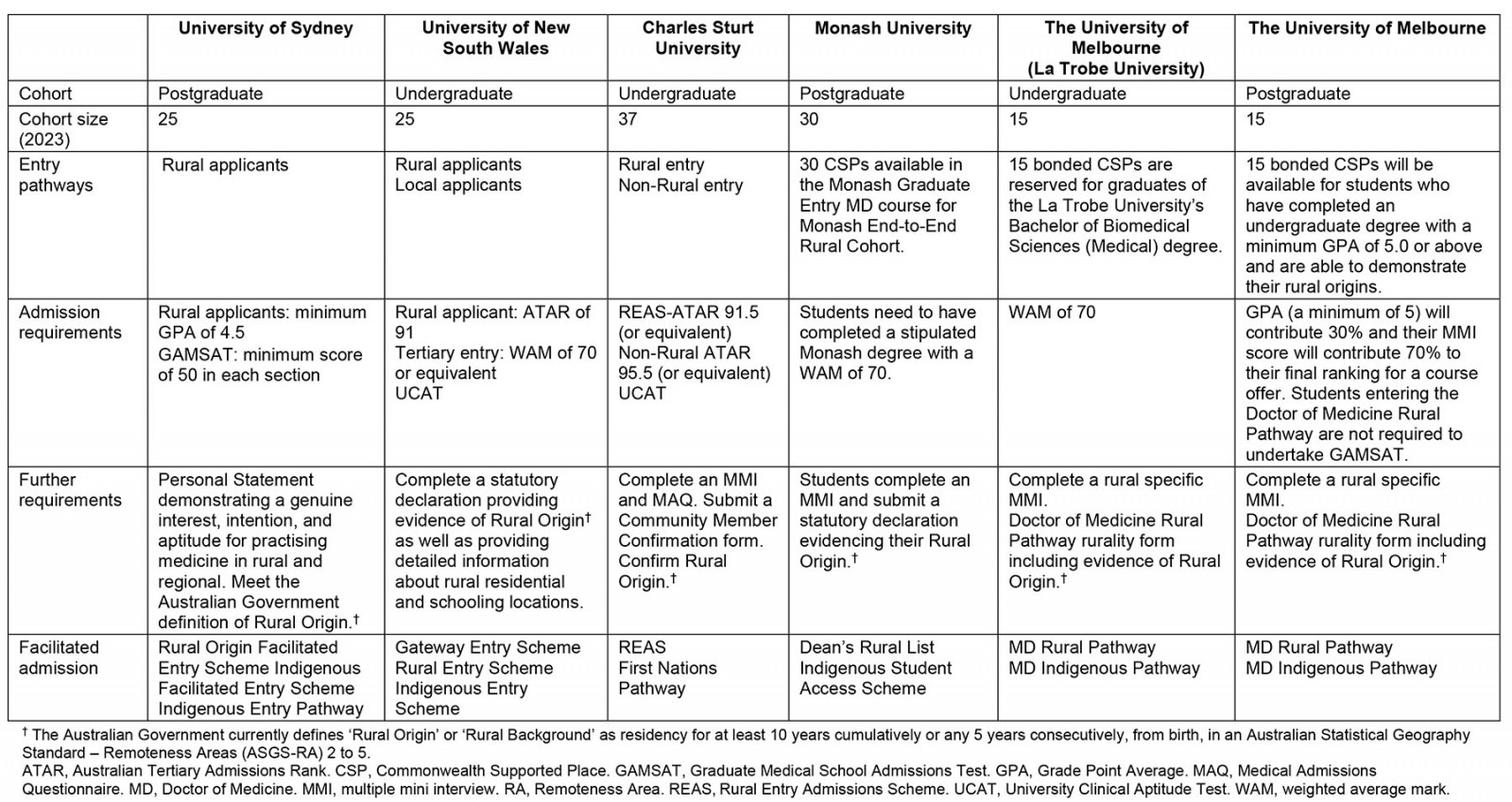
Data collection
Each medical program will collect its own administrative, survey and registration data as relevant to the study objectives (Fig2). Data consistency will be maintained through the use of a data dictionary and standardised survey instruments. Australian medical graduates receive a medical registration number from the regulator, the Australian Health Practitioners Regulatory Agency (Ahpra), following graduation; prior to this, student identification number is the primary means of student identification. Participant confidentiality will be maintained through the de-identification of all research data and allocation of a random participant identifier. Only the chief investigator and project officer for each university will have access to the code used to link respondents’ student identification numbers or medical registration numbers with their random participant identifier. De-identified aggregate data will be held in a central repository. A data custodian has been appointed to oversee the management and security of these data.
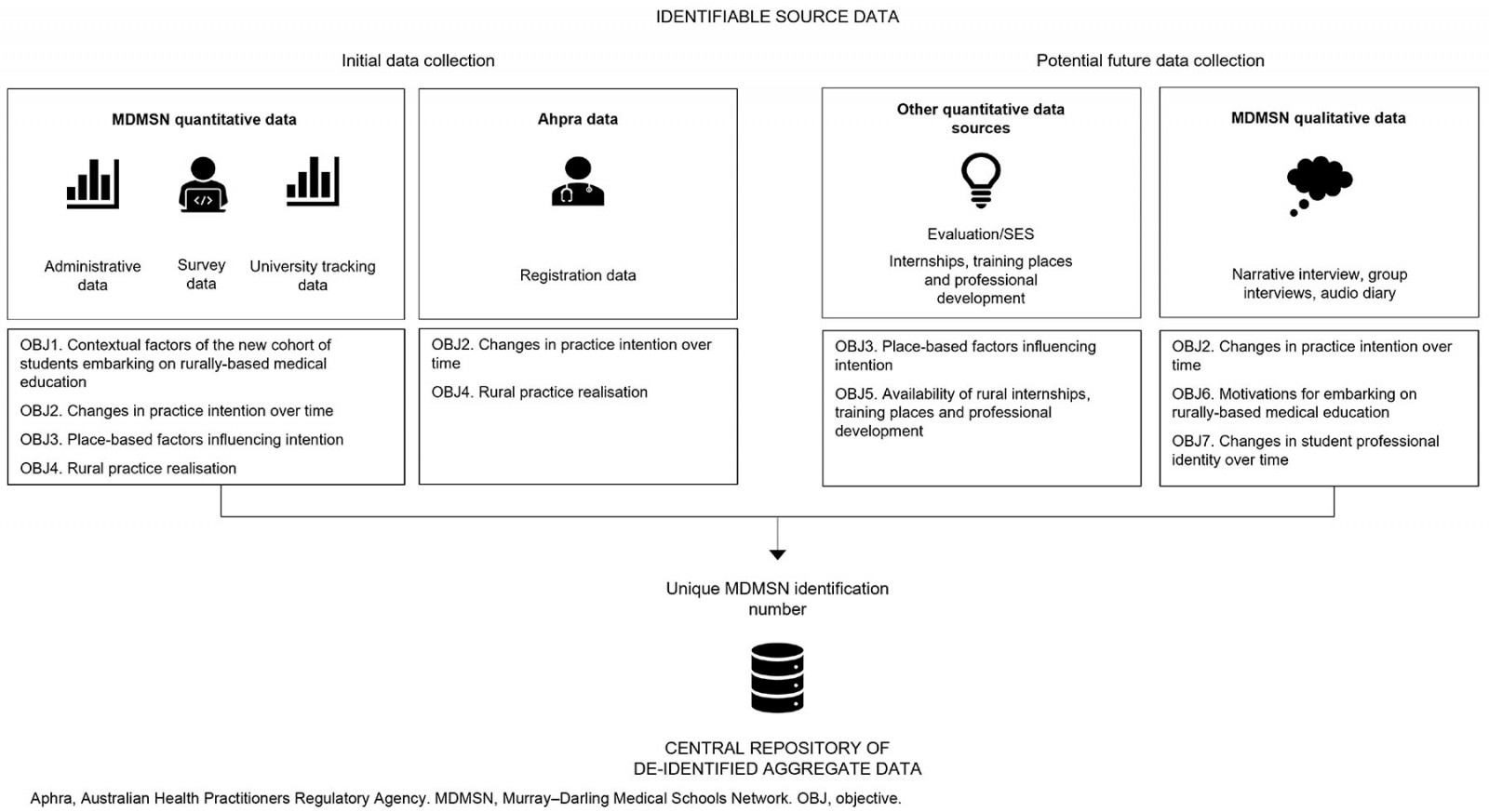 Figure 2: Components of data collection in relation to the study objectives.
Figure 2: Components of data collection in relation to the study objectives.
Administrative data: Administrative student data (admissions, enrolments and completions) will be collected from existing university datasets. Key demographics of interest include sex, age, marital status, indigeneity, country of birth and student status (domestic or international).
Survey data: Collaborators from each respective university will distribute an entry survey to all first-year students undertaking rurally based medical programs. The entry survey will collect demographic information as well as information regarding rural background, students’ journeys to medicine, preferences, and future practice intention (Table 2). The survey instrument has been carefully designed to collect only information that is not available from other sources (eg administrative data). Survey questions have been aligned with and adapted from the Medical Schools Outcomes Database survey7, the Australian Bureau of Statistics, and from the literature with permission from the authors5.
Table 2: Entry survey for the Murray–Darling Medical Schools Network research collaboration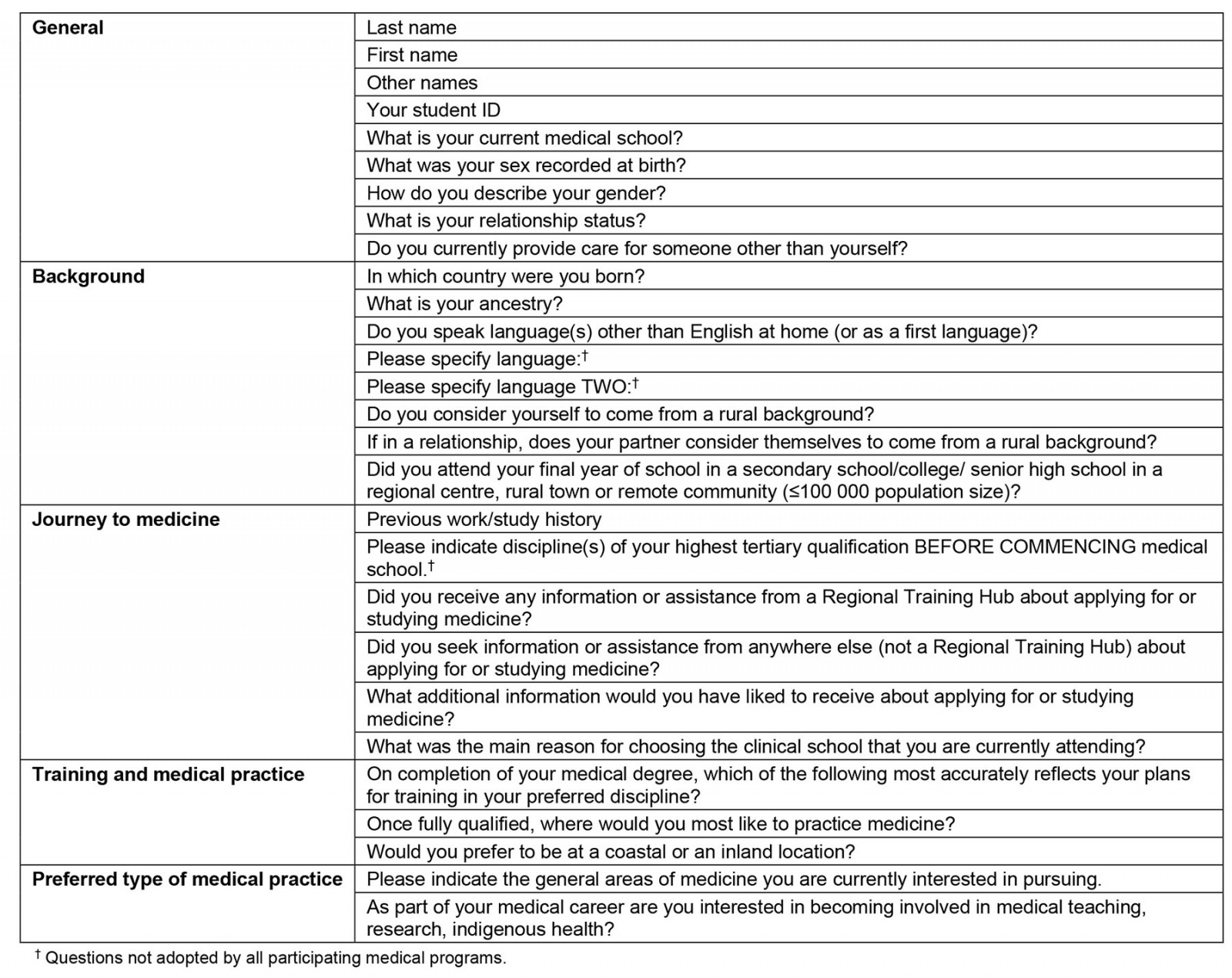
University tracking data: University-level graduate tracking data will also be collected by individual university partners. Potential data sources include state-based postgraduate medical councils, the Medical Schools Outcomes Database and alumni. Other quantitative data sources may involve student experience surveys or data on medical internships, training places and professional development.
Registration data: Registration data will be collected from Ahpra. Medical practitioners are required to be registered to practice in Australia, and Ahpra is the single national registration authority. Ahpra maintains and publishes an online database including an annual update of practitioners’ principal place of practice and specialist registration. Rurality of location will be determined using the Modified Monash Model geographical classifications21.
Data analysis
Descriptive statistics will be used to summarise survey results. Analyses will be undertaken to explore interrelationships among survey responses. Comparative statistics will compare survey results and future practice location between successive cohorts of the five medical schools in the MDMSN.
Ethics approval
Ethics approval was obtained from the University of Sydney Human Research Ethics Committee (HREC; ref. no. 2022/015). Lead HREC approval was ratified by all partner university HREC. University-held student personal information (eg administrative student data) will be used in accordance with each university’s policies, procedures and HREC approvals.
Results
Participating medical programs are responsible for collecting their own internal university survey and registration data as relevant to the study, and will provide access to de-identified data related to their own students and graduates. In the short term, the MDMSN research collaboration will focus on the rural cohort, not surveying the entire cohort where there are metropolitan schools, and on deep dives rather than large-scale quantitative analyses. However, it is hoped that meaningful comparison with the existing system of extended rural clinical school placement and between rural and metropolitan cohorts will also be possible in future. Longer term, the group will work towards the development of a central repository of de-identified aggregate data designed to increase the power of the data collection and the potential for the group to co-design research of national relevance. In the first instance, access to de-identified data in the aggregate dataset will be granted only to those university partners named in the ethics application. This may be modified in future with approval from the lead HREC. To support research capacity building in rural areas, the MDMSN research collaboration is also exploring the possibility of cross-collaborative higher degree research projects.
Discussion
Health workforce maldistribution in rural and remote areas relative to metropolitan cities is a global issue that can compound pre-existing geographical and socioeconomic disadvantage, leading to poorer health outcomes in these communities24. Policymakers and educators have taken a multifaceted approach to strategies designed to increase the recruitment and retention of a rural health workforce25. However, the scope of the challenges faced, including the availability of a skilled and motivated workforce, is broad24. One potential solution is to provide medical education to students in place (eg in rural areas).
Until recently, there were only a small number of universities in Australia in which students could undertake the entirety of their medical degree in a regional or rural area. These include James Cook University (JCU) in North Queensland26, the Flinders University Northern Territory Medical Program27 and the University of New South Wales in Port Macquarie. However, with the expansion of rurally based medical programs a new rural pipeline is emerging. JCU Medical School, established in 2000, has accumulated the most evidence in this area26. In 2019, it was reported that just under half of JCU medical graduates (46.1%, postgraduate years 5–14) were working in a regional, rural or remote area28. JCU also employs a number of initiatives to encourage graduates to practise rurally, including an extended rural clinical school program, integrated rural placement and Longitudinal Integrated Clerkship28. The Flinders University Northern Territory Medical Program, a younger program that commenced in January 2011, also reports a high retention rate in (73.2%, MM 2–7), with just over half of all graduates in working in MM 2 (mostly in Darwin). The program includes a 2-year return of service obligation, which further extends the rural immersion of this cohort but also makes direct comparisons difficult29.
The immediate focus of the MDMSN research collaboration is on the first two engagement points in the rural pipeline. However, it is important to acknowledge that rural background and rural medical education form only part of the possible pipeline to subsequent rural practice. More work is also needed to improve the availability of rural vocational medical training and continuous professional development for rural health workers. This work is commensurate with the roles of the RMHT funded Regional Training Hubs, which work with Local Health Districts, medical students and rural Doctors in Training to support rural medical workforce development. In time, systemic shifts in prevocational and vocational training pathways such as the implementation of the new John Flynn Placement Program and the shift to college-led training in general practice, among others, will also influence career opportunities for graduates of these rurally based medical programs. The MDMSN research collaboration is working to remain aware and responsive to the milieu of personal, contextual and place-based factors that influence postgraduation decision-making at the level of the individual but sit outside of the scope of the current study. This collaboration will seek further engagement with Regional Training Hubs as part of potential future progression of this work.
Limitations
The limitations of longitudinal programs such as this have been discussed previously10 and are also relevant to this work. Initially, the main limitation for the MDMSN research collaboration will be the size of the cohort. The authors concede that numbers are small within each of the individual medical programs. Nationally, the rural cohort is small in comparison with its metropolitan counterparts. Participating medical programs also differ in their entry requirements and school level demographics. It is for this reason, however, that it is imperative for collaborations such as the MDMSN research collaboration to produce more solid evidence through combined effort, both across institutions and longitudinally. Other potential challenges associated with long-term collaborative programs include the ability to ensure consistent data collection methods across universities to maintain reliability and validity of data, difficulty in sustaining the commitment of university partners, and facilitating productive collaboration among diverse stakeholders with varying interests and priorities. To date these challenges have not been an issue. Minor, program-specific variations in the entry survey have been negotiated and recorded, and the enthusiasm of the group is high. A quorum of a least one member from each medical program is requested at meetings as per the terms of reference for the group; however, most meetings are attended by two or three members from each program, demonstrating an ongoing commitment to working together. Data fragmentation and accuracy, governance and managing loss to follow-up will be elements of ongoing focus for the collaboration.
Over-surveying of medical students in general, and rural medical students in particular, is known to be an issue at both a local and national level. The formation of a cross-MDMSN student advisory group is one strategy employed by the collaboration to assist with loss to follow-up. These students will represent their cohort throughout their medical degree, increasing student engagement by providing results to other students and feedback to the research team to guide the development to the project. Considerable effort was also made to ensure that the entry survey was aligned with other existing survey instruments such as the Medical Schools Outcomes Database survey to allow for suitable comparison and possible future collaboration.
In addition to the quantitative longitudinal work, qualitative research programs are being undertaken by individual university partners (eg narrative interviews, group interviews and audio diaries)30,31. It is proposed that these programs will be aligned in future. However, a consistent methodology that can be implemented by all partner universities requires further time and consideration. The coordinated collection of qualitative data has considerable challenges but will be invaluable for the realisation of potential future research objectives.
Conclusion
The partner universities in the MDMSN research collaboration form a diverse, multi-institutional team that is working to maximise the unique opportunity provided by the MDMSN program. The group is taking a combined, longitudinal approach to explore medical training capacity in the Murray–Darling region by developing an evidence base with which to undertake research of national relevance and to inform and influence policy and practice. Although initial efforts are focused on understanding the new cohort of students embarking on rurally based medical education, there is enormous scope to expand this research to gain a deeper understanding of the rural student experience, the effect of place, development of professional identity, and relationship to subsequent rural practice. The ultimate goal of the MDMSN research collaboration is to work together to help grow the rural medical workforce.
Acknowledgements
The authors thank Professor Catherine Hawke, a member of the MDMSN research collaboration, for critical review of the study protocol. We also thank academic and professional staff from all participating universities, including the Regional Training Hubs.
Funding
The partner universities are funded by the Australian Government under the Murray–Darling Medical Schools Network.
Conflicts of interest
The authors declare no conflicts of interest.











