Introduction
The accelerated process of population aging has gained evidence in Brazil and other low- and middle-income countries1. The increasing number of older adults in these countries has demanded greater care to prevent diseases and maintain the health of aging populations1,2. In rural Brazil, population aging is characterized by higher proportion of men than women3,4, low income3, precarious living5,6 and limited access to health care7.
Sarcopenia is related to the aging process and leads to a decline in the musculoskeletal system, leading to adverse health outcomes and higher health system costs8. One of the main research groups in this field, the European Working Group on Sarcopenia in Older People (EWGSOP), recommended the use of three different combinations of muscle assessment to diagnose sarcopenia (muscle mass, strength, and performance), with low muscle mass being the main criterion for diagnosing the disease9. An update made by EWGSOP28, in 2019, recognized low muscle strength as the main criterion for identifying probable sarcopenia, and, when considered together with low muscle mass, diagnosis of the disease is confirmed. In addition, the group advised that, in order to assess the severity of sarcopenia, muscle performance should be evaluated, considering sarcopenia to be severe when muscle performance is low8.
The group8 also recommends using the Find-Access-Confirm-Severity (FACS) algorithm to identify and confirm sarcopenia cases. Screening begins with the Strength, Assistance with walking, Rising from a Chair, Climbing stairs, and Falls (SARC-F) questionnaire, followed by the analysis of the other criteria8. However, the validity of the SARC-F questionnaire has been questioned in the literature10. EWGSOP2 recognized its low sensitivity and moderate–high specificity, detecting primarily severe cases8. Recently, a meta-analysis demonstrated the inappropriateness of this test for sarcopenia screening10.
Recent updates and inconsistencies in the identification of sarcopenia have impacted the prevalence of sarcopenia in Brazil and worldwide. According to the EWGSOP2 criteria, sarcopenia prevalence ranges from 0.8% to 28%11-14. In Brazil, prevalence varies from 10.1% to 33.7%15,16 and, when other assessment criteria are used, prevalence varies from 1.9% to 33.3%17-19.
Despite these differences, the impact of sarcopenia is considerable8,9,15,20. Falls, fractures, functional disability, hospitalization, and mortality are some of the factors associated with sarcopenia8,9,20.
Considering the accelerated ageing process and the limited knowledge about the burden of sarcopenia and its consequences among older adults living in rural areas, this study aimed to estimate the prevalence of probable sarcopenia and its associated factors using EWGSOP2 criteria.
Methods
This cross-sectional study using data from a prospective cohort, the EpiRural Cohort Study, aimed to describe and monitor patterns of morbidity and mortality and the use of health services by older people (aged ≥60 years) living in the rural area of the municipality of Rio Grande, in Rio Grande do Sul State, Brazil. Rio Grande is a municipality located in southern Brazil and, in 2017, its population was estimated as being 209 378 inhabitants, of whom approximately 5% lived in rural areas2,3. The rural area of Rio Grande is delimited by the Laguna dos Patos, the Atlantic Ocean and Laguna Mirim water bodies, where traditional communities live mainly from fishing and family farming, including livestock, rice and soybean. The baseline data were collected in 2017, when 1029 older adults were identified through mapping and a random selection of permanently inhabited households in the rural area of the municipality. The first follow-up was conducted between 2018 and 2019 with the participation of 862 older adults (available from authors upon request). Further information about the EpiRural Cohort Study can be found elsewhere21.
The EpiRural's second follow-up was conducted between November 2020 and January 2022 (with unpredicted interruptions due to the COVID-19 pandemic). Two structured questionnaires were applied through face-to-face home interviews conducted by trained interviewers, accompanied by a field supervisor. Information was collected about sociodemographic, family, behavioral, and health characteristics of the older adults. Data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at the Federal University of Rio Grande22.Probable sarcopenia was assessed using a handgrip strength test (HGS) performed with a Saehan hydraulic dynamometer, following the current standards8,23,24. The HGS test was performed with the older adults seated in an armless chair without a back support, legs together, and feet on the floor, with the elbows in a position close to the body at 90º of flexion24. In this position, the dynamometer was handed over to the participants and, after adjustment to the correct hand size, the older adults were asked to squeeze the equipment for 5 s with maximum force. The other hand remained in a neutral and relaxed position, resting on the opposite leg to which the HGS test was being applied. Three measurements were taken for each hand, starting with the right and then the left hand, with an interval of approximately 30 s of rest between each measurement25. For analytical purposes, the highest measurement of the six was considered. The dependent variable, probable sarcopenia, was operationalized as the presence of low HGS, according to EWGSOP28. The cut-off point for low muscle strength is HGS <27 kg for men and <16 kg for women8,26.
The following independent variables were examined: sex (male/female), age (60–69 years; 70–79 years; ≥80 years), body mass index (BMI) (underweight: ≤22 kg/m2; healthy weight: 22–27 kg/m2; overweight: ≥27 kg/m2)27, smoking status (never smoked; current smoker; former smoker), presence of self-reported diseases (hypertension (no/yes); diabetes mellitus (DM) (no/yes); chronic obstructive pulmonary disease (COPD) [no/yes) that was considered as the sum of the following self-reported diseases: asthma, bronchitis, emphysema; depression (measured with the Patient Health Questionnaire-9 (PHQ-9) (no/yes)), presence of spinal pain (no/yes) (considered as the sum of pain in the cervical, thoracic and lumbar regions of the spine), presence of knee pain (no/yes), and hospitalization in the previous 12 months (no/yes).
Data collection during the COVID-19 pandemic was performed following all social and sanitary norms.
Initially, a descriptive analysis of the data was conducted to identify the main characteristics of the older adults. The Shapiro–Wilk test was performed to assess the distribution of continuous data, and the symmetry of the distribution. Continuous variables were tested using the Mann–Whitney U-test. Prevalence of the outcome according to the independent variables was examined using the χ² test. Factors associated with probable sarcopenia were examined using crude and adjusted Poisson regression analysis. The adjusted analysis followed a hierarchical model controlling for confounding factors: first level (sex and age), second level (BMI and smoking status), third level (self-reported diagnosis of hypertension, DM, depression, COPD, presence of back pain, and presence of knee pain), and fourth level (hospitalization in the previous year). Variables with p<0.20 were kept in the model and a 5% significance level was adopted.
Ethics approval
This research was approved by the Research Ethics Committee of the Health Area of the Federal University of Rio Grande through Opinions No. 51/2017 and No. 154/2018. All ethical aspects were observed in accordance with National Health Council Resolution No. 466/12. Participation was voluntary, and all participants provided free, prior and informed consent.
Results
A total of 651 older adults were followed up in the second wave of the EpiRural Cohort Study in Rio Grande. We found that 51.9% were male, 45.8% were aged 70–79 years, and the majority (50.7%) were overweight (BMI ≥27 kg/m2). Among the diseases investigated, 59.7% of the participants self-reported hypertension, 15.0% DM, 17.4% COPD, and 7.1% depression (Table 1).
Prevalence of probable sarcopenia was 19.2% (95% confidence interval (CI) 16.3–22.5%). Occurrence of probable sarcopenia was higher among males (23.8% v 14.3%) and increased with age, reaching 44.3% in adults aged ≥80 years. Prevalence of probable sarcopenia was higher among older adults with diabetes (28.6%), depression (30.9%) and those who had been hospitalized in the previous year (41.4%) (Table 2).
Mean HGS was 27.8 kg (standard deviation (SD)±9.33), and males had a higher average (33.1±8.58 kg) than females (22.1±6.25 kg) (Table 3).
In the adjusted analysis, there was a linear gradient between age and probable sarcopenia, with those aged ≥80 years having a 4.15 times greater risk higher compared to those aged 60–70 years (prevalance ratio (PR) 4.15; 95%CI 2.65–6.50). In addition, there was association with the male sex (PR 1.61; 95%CI 1.17–2.21), underweight (BMI ≤22 kg/m2) (PR 1.90; 95%CI 1.23–2.93) in comparison to healthy weight individuals, diabetes mellitus (PR 1.80; 95%CI 1.20–2.73), and hospitalization in the previous year (PR 2.00; 95%CI 1.36–2.91) (Table 4).
Table 1: Characteristics of a sample of older adults living in the rural area of Rio Grande do Sul State, Brazil, 2020–2022 (n=651)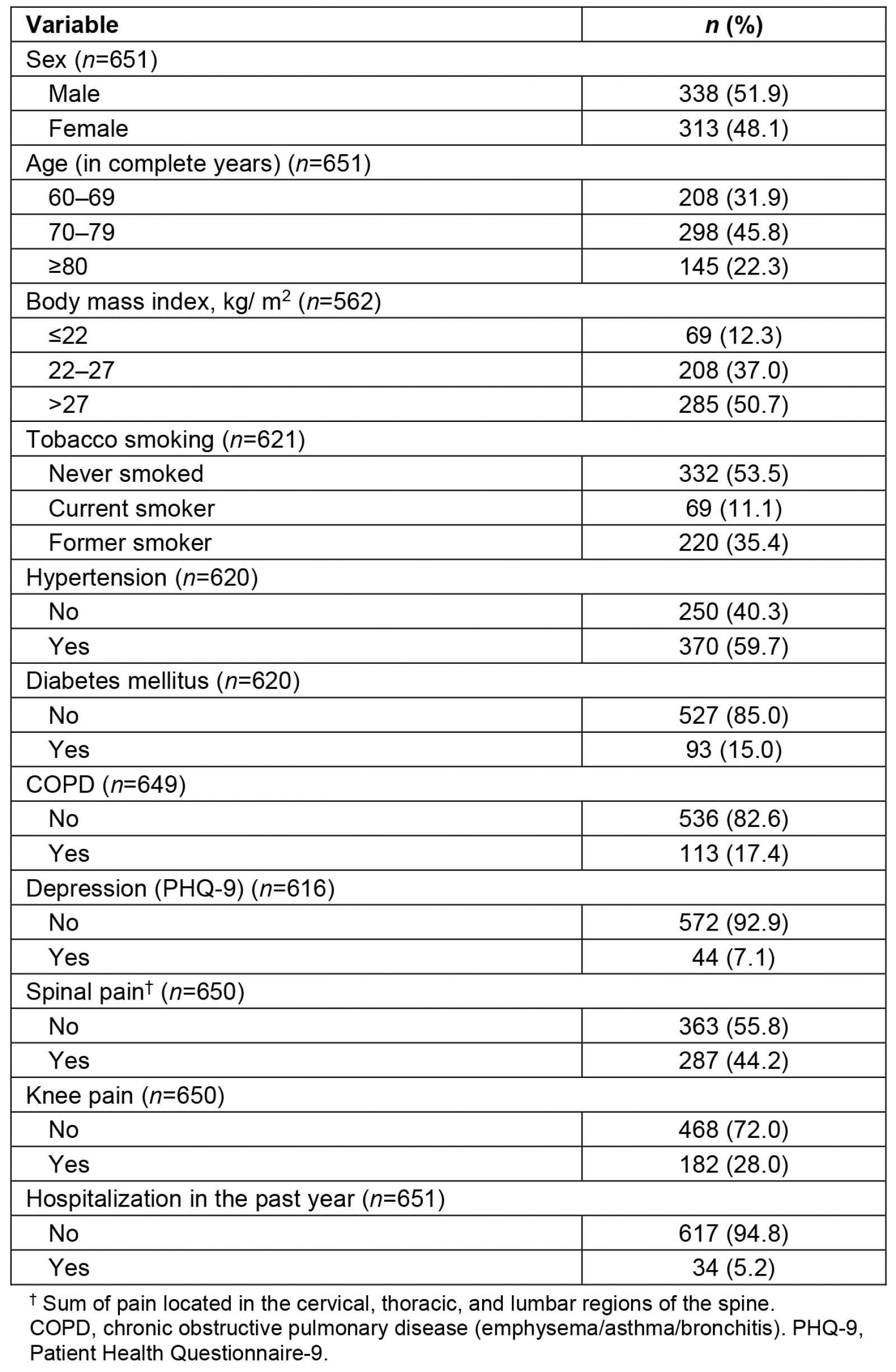
Table 2: Prevalence of probable sarcopenia, according to independent variables, in the rural area of Rio Grande do Sul State, Brazil, 2020–2022 (n=624)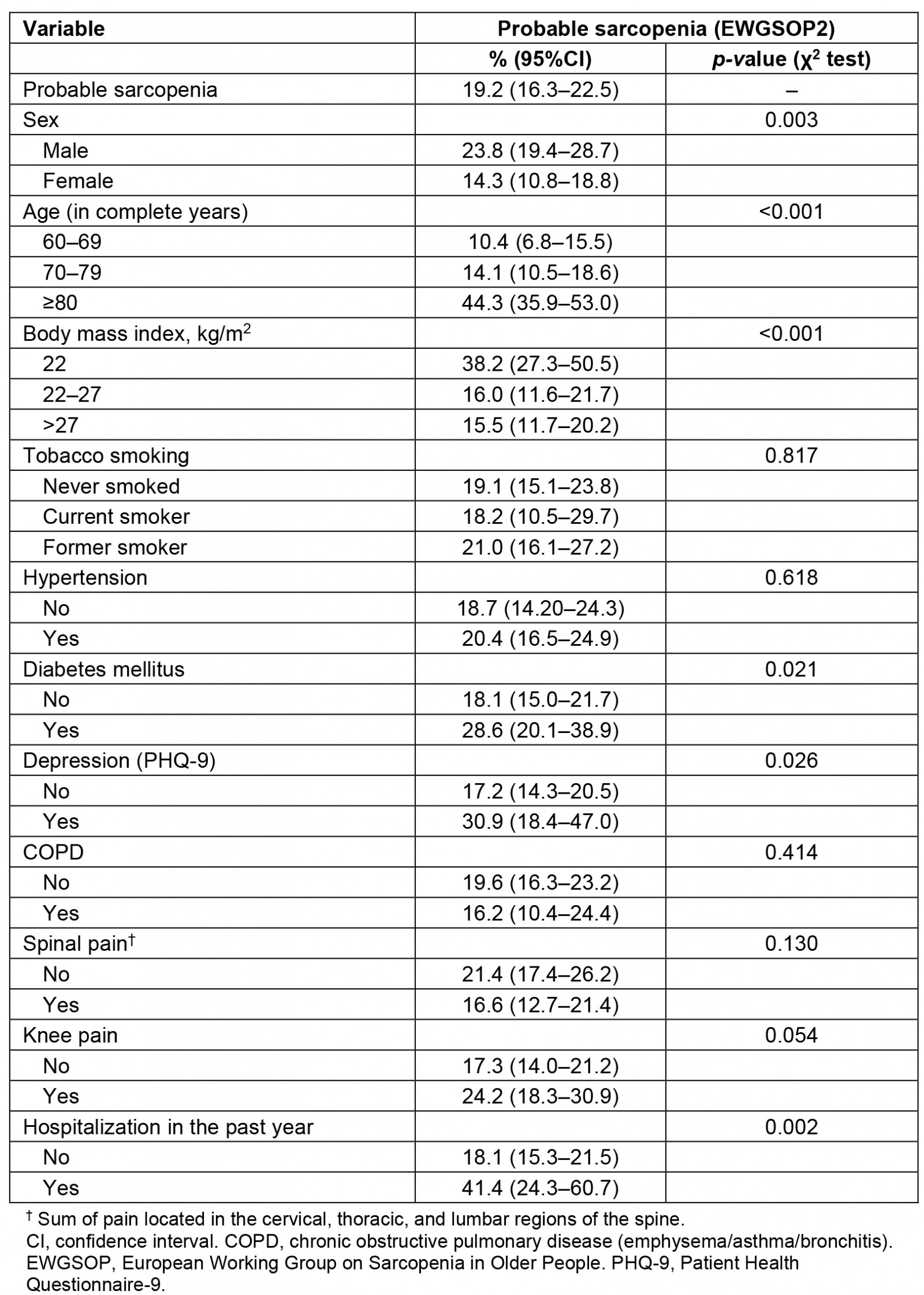
Table 3: Mean, standard deviation and median measurements of handgrip strength, calf circumference and gait speed of older adults living in the rural area of Rio Grande do Sul State, Brazil, 2020–2022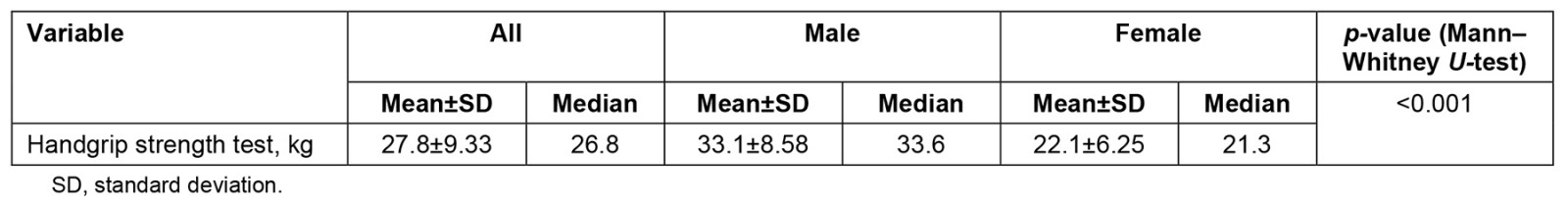
Table 4: Crude and adjusted analysis of associations between prevalence of probable sarcopenia (EWGSOP2) and independent variables, rural area of Rio Grande do Sul State, Brazil, 2020–2022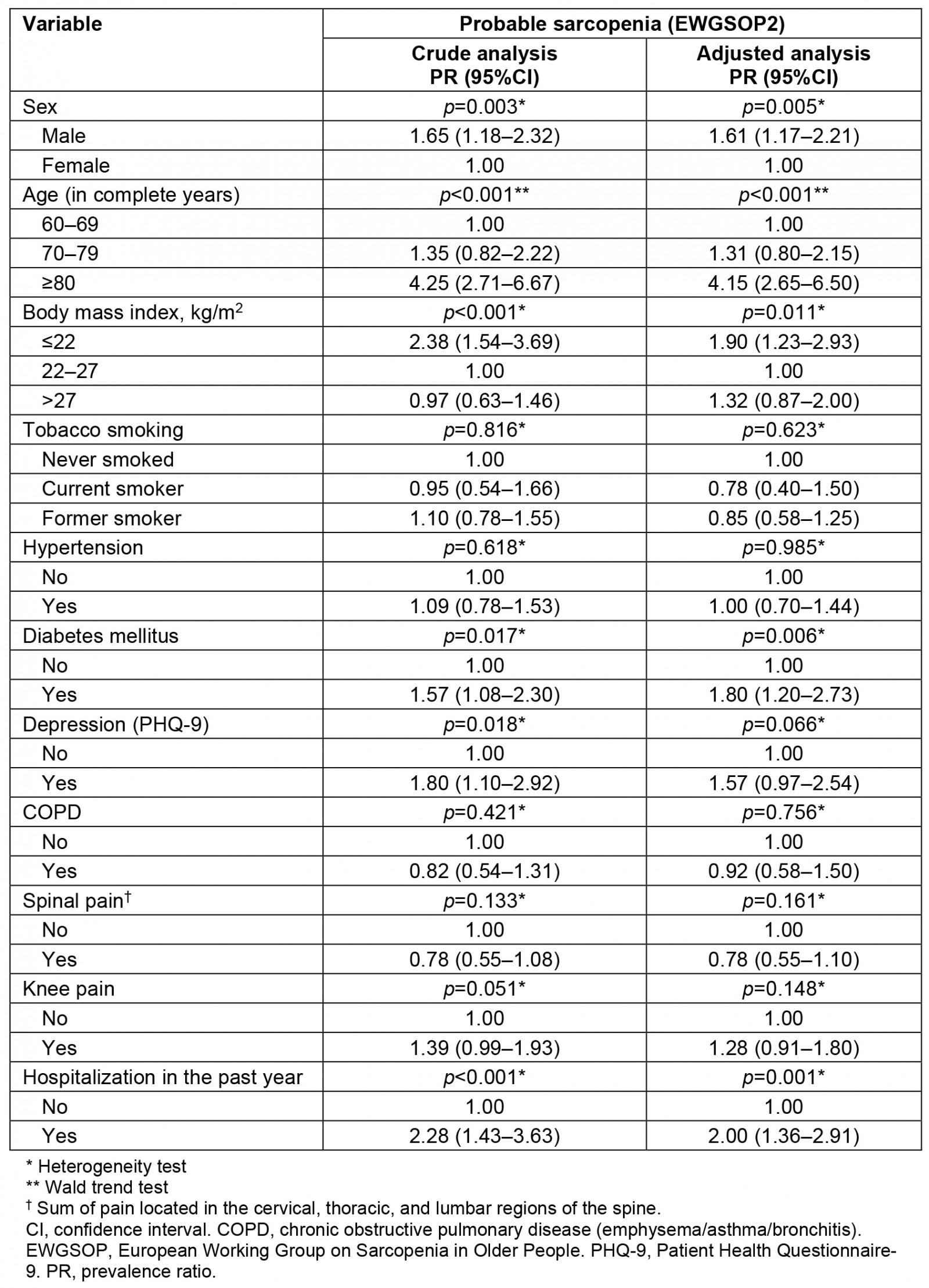
Discussion
This study found that one in five older adults living in rural areas in the far south of Brazil has probable sarcopenia. Male sex, age ≥80 years, underweight, having DM and having been hospitalized in the previous year were associated with the outcome.
In Brazil, few population-based studies have assessed probable sarcopenia and only one reported similar prevalence to our findings15. Similar results were observed in Asia in a study of older adults living in urban and rural areas14. In Europe, prevalence of probable sarcopenia is higher than that reported in Brazil11,15,28,29. There are few studies analyzing the differences in the occurrence of probable sarcopenia between areas of residence (urban v rural). However, rural prevalence of sarcopenia in older adults has great variability30-32 and these divergences may be related to recent updates of sarcopenia criteria.
One unexpected finding of our study was that males have a higher risk of probable sarcopenia than females, contradicting previous studies suggesting that females in Latin America are at a greater risk of sarcopenia33, including a Peruvian study carried out only with older adults living in rural areas32. In Portugal, protection for males was identified using the EWGSOP2 criteria for diagnosis of sarcopenia (odds ratio (OR) 0.52 (0.29–0.97))29.
Another Brazilian study found similar results but using different diagnosis criteria19. In southern Iran, males are also at higher risk of sarcopenia (OR 3.13 (91.23–7.98)34. This may possibly be due to the high cut-off point indicated by EWGSOP2 to consider low muscle strength in men, which is much higher than that applied in women, leading to an overestimation of probable sarcopenia in men. A recent Brazilian study suggested a lower HGS cutoff for men35, which may be more reliable in relation to the Brazilian population. Therefore, new studies with other HGS cut-off points for males are needed to confirm or refute this association. Another possible explanation is the fact that male are more likely to develop work-related injuries in rural and fishing activities.
Association between aging and probable sarcopenia has also been found in studies that used the updated EWGSOP2 criteria12,29 and studies using several other criteria19,30,32,33. This can be explained by the natural process of body aging that involves increased protein degradation, changes in body composition, increased fat infiltration into muscle tissue, increased inflammatory cytokines, decreased body homeostasis, and decreased circulating hormones, which contributes to the risk of sarcopenia36,37. Notably, older people aged 70–79 years were not at risk of probable sarcopenia. This finding can be explained by the fact that some older adults remain active and perform activities that require greater physical effort on their rural properties, with less sedentary behavior when compared to older adults living in urban areas38. Another possible explanation can be the peculiarity verified in the most recent Brazilian agricultural census (2017)3, in which 23% of rural producers were ≥65 years old3, suggesting that a large proportion of Brazilian older adult residents in these locations participate in the productive scenario in the Brazilian countryside.
Several studies conducted in Brazil and worldwide have reported association between underweight and sarcopenia14,19,30,34,39. The BMI measurement is easily performed in both clinical practice and population-based studies, and is considered a reliable indicator of nutritional status in older adults27,40. Although there are differences in the cut-off points for BMI in older adults40,41, the literature is consistent with the assumption that underweight in the older adults should be monitored frequently, as it increases the risk of malnutrition, and consequently the impairment of health, increasing the risk of sarcopenia, frailty, vulnerability, and mortality41.
The association of diabetes mellitus with probable sarcopenia observed in our study (PR 1.89 (1.30–2.75)) was also found in studies performed in Asia42 and Europe43. A recent meta-analysis of observational studies found that one disease leads to another, especially in individuals who already have DM complications44. Some of the pathophysiological mechanisms of DM also occur in sarcopenia, including increased insulin resistance, chronic inflammation, and mitochondrial changes45. In addition, Park et al (2006)46 identified that older adults with DM have lower muscle strength. However, our research did not analyze the type of DM (type I or II), time of disease onset, or use of specific medications, which are suggestions for future research.
Association between probable sarcopenia and hospitalization in the previous year is well established in the literature8,20,47. Hospitalization leads to decreased muscle strength and mobility, mainly because of the negative effects of a long stay in hospital beds, which can increase the risk of sarcopenia among the older adults, especially those affected by comorbidities43,47,48. Thus, hospitalization is an important risk factor, suggesting the need for intervention during and after this period, increasing body mobility and encouraging performance of guided exercises.
However, this study had some limitations. Its cross-sectional design presents a reverse causality bias, which makes it impossible to establish a cause-and-effect mechanism between the associations, especially in relation to BMI. Additionally, information on level of physical activity, cognitive impairment and quality of life in the older adult participants was not collected, making this analysis unfeasible. Lastly, some health information may be biased since it was self-reported.
Among its strengths, our study followed the EWGSOP2 updates to diagnose probable sarcopenia, being, to the best of our knowledge, the first Brazilian population-based study to measure the occurrence of sarcopenia by applying these criteria to older adults living in a rural area. We believe that EWGSOP2 enhances our comparability with the literature. In addition, the easy use of a dynamometer, and its low cost, make it a feasible resource for clinical practice of primary health care, facilitating access to screening probable sarcopenia, and initiating necessary interventions as early as possible8,49,50. We suggest further research on sarcopenia in rural populations.
Conclusion
Probable sarcopenia can easily be identified in primary health care and reversed through specific health care. Older adults living in rural areas require especial attention, particularly males, individuals aged ≥80 years, underweight, diabetics and those hospitalized in the previous year.
In addition, we highlight the importance of having more health professionals working directly in musculoskeletal health care, as well as investment in facilities for health promotion and engagement in resistance exercise programs, allied with changes in lifestyle that can support reversing the condition of probable sarcopenia and minimize its impact on older adults’ health.
Finally, we believe that our findings can contribute to directing public health policies for older adults by investing in the prevention of probable sarcopenia.
Funding
The authors acknowledge the Research Support Foundation of Rio Grande do Sul (FAPERGS).
Conflicts of interest
The authors declare that there is no conflict of interest.




