Introduction
Evidence suggests that improving trust in doctors could assist in addressing challenges associated with patient healthcare service uptake, compliance and continuing engagement with care, particularly among those with non-communicable diseases. A high level of patient trust in doctors is reported to improve biomedical healthcare seeking and use1-3, reduce risky behaviours and increase medication adherence4-7, continuity with care8,9 and disease control4,6,9. Therefore, much of the current literature concerning trust in therapeutic relationships has focused on factors that shape patients’ trust in doctors in primary healthcare settings10-21. Existing research has facilitated the design and testing of trust improvement interventions22,23 and generated a number of measures of patient trust in high-income countries24-28. However, most studies on factors shaping patent trust in doctors, especially those related to doctors’ trustworthiness, have been conducted in urban settings in high-income countries. Although the health service delivery, cultural norms and patient expectations in typical rural low-income Africa differ from those in high-income countries, factors shaping doctors’ trustworthiness have not been examined in this context. This study draws on the perspectives of patients in rural Tanzania to examine the factors that shape doctors’ trustworthiness in the context of hypertension care. This will provide much-needed information for designing and testing trust improvement interventions in rural low-income Africa.
Methods
The methods used in this study have been reported elsewhere29. In summary, this article is based on a qualitative study that sought to examine the meaning, benefit and factors shaping patient trust in doctors in rural Tanzania29. Tanzania was selected as it is a unique rural low-income Africa setting30. Tanzania also has a rapidly growing burden of non-communicable diseases characterised by poor patient healthcare seeking, non-adherence, poor continuity with care and poor disease control31-35. Hypertension was chosen as the exemplar because of the lengthy patient–doctor interactions required during hypertension management. The study from which the present data were drawn was conducted in 12 health facilities in two predominantly rural districts of Shinyanga region, Tanzania, between October 2015 and March 2016.
Participants were purposively sampled and recruited via verbal advertisements during health education sessions and institutional meetings, and through peer referrals. Purposive sampling was used because statistical representation was not the primary goal36. During participant recruitment, no strict inclusion criteria were applied other than the inclusion of patients who were seeking hypertension care at the time this study was conducted. Interviews with participants were conducted in quiet, isolated rooms that were disconnected from regular clinics in the participating health facilities. The interviews were audio-taped with participants’ consent. Data were gathered using a flexible interview guide that covered the perceived meaning and benefits of trust, and factors shaping patient trust in doctors. A consultative process involving experts in both Tanzania and Australia was used to develop and translate the interview guide into Swahili. Before the interviews, each participant was given an information sheet and a verbal description of the study in Swahili, and their verbal consent was obtained and recorded. The duration of each interview was approximately 45 minutes.
Data transcription and translation occurred simultaneously. After transcription and translation, the interview transcripts were de-identified, and pseudonyms were generated for each participant. The data were uploaded into NVivo v11 software (QSR International; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home) for thematic coding. The thematic analysis was based on the approach described by Braun and Clarke37, and began after the first few interviews and continued as more data were gathered. Specifically, the first author (KI) generated initial codes from the data extracts of the first three transcripts. Then, these codes were reviewed by the research team (NS, HS, TN, RJ) to generate a list based on consensus. KI continued coding the rest of transcripts, and refined and generated more codes upon coming across new segments of data that did not fit into the initial codes. Coding of transcripts continued throughout data collection until no new information was generated from the interviews. Codes were then sorted into potential subthemes and themes, followed by collation of all relevant coded data extracts into identified themes. Throughout this process of coding and refinement, the research team held frequent discussions to reflect on the themes generated. This peer consultation also aimed to address potential bias that might have resulted from KI’s interpretation of the data, as that author is a medical doctor in the country where the research was conducted. Patients’ accounts of provider factors that shaped their trustworthiness were used for this analysis.
Ethics approval
This study received ethics approval from the Human Research Ethics Committee at the University of New South Wales, Australia (HC15535) and the National Institute for Medical Research, Tanzania (NIMR/HQ/R.8a/Vol. IX/2024). Authorisation was also obtained from local health authorities.
Results
In total, 34 patients aged 34–75 years (average age 53.3 years) receiving Western-based hypertension care were recruited for this study (28 women and 6 men). Most participants identified as Sukuma. Participants included healthcare workers (32.4%) and non-healthcare workers (67.6%), such as farmers (26.5%) and other occupations. Table 1 summarises participants’ characteristics.
There was broad consensus among participants on factors that shaped doctors’ trustworthiness in rural Tanzania. Variations in participants’ narratives related to when each factor was perceived as shaping doctors’ trustworthiness along the trajectory of care (i.e. before, during and after a therapeutic encounter).
Table 1: Participant demographics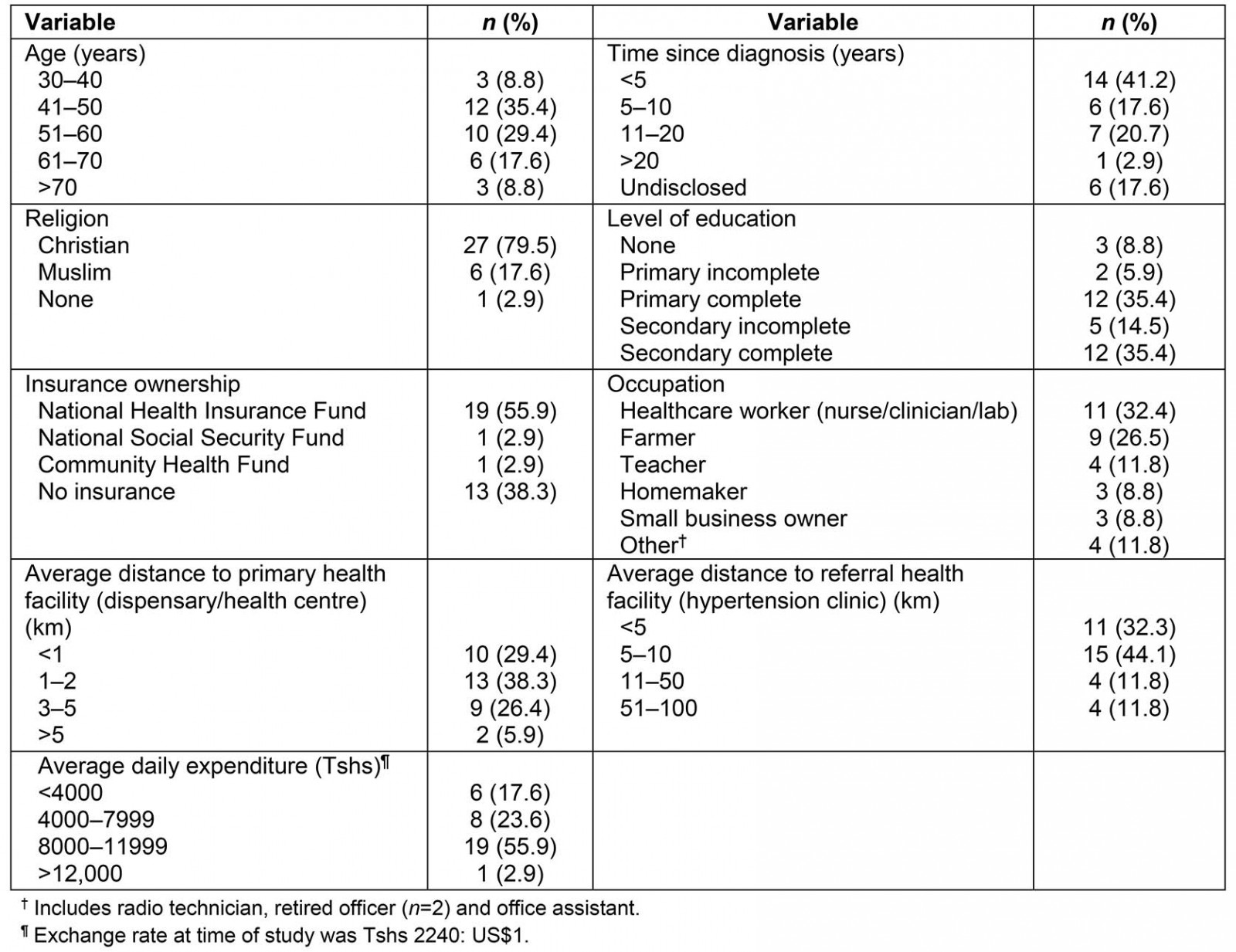
Factors shaping doctors’ trustworthiness before a therapeutic encounter
Many participants indicated that a doctor’s behavioural and technical reputation within their community/social networks and among other patients were important factors that shaped trustworthiness. Some described actively and passively receiving information about and recommendations for a good (trustworthy) doctor from family, friends or neighbours before seeking care. For example, Urio (teacher) said:
… Information about the reputation of doctors spread in the community. I often ask my friends who is a good doctor and whether he is available on the day I want to visit. That way I find myself having initial trust towards the doctor before even talking to him.
Information about a doctor being ‘good’ or ‘bad’ was also obtained from other patients when queuing to encounter a doctor at a healthcare facility or hypertension clinic. Queuing to encounter a doctor was described as customary in the study settings. Mlasi (homemaker) said:
You may overhear [other] patients talking that [a certain doctor] always treat patients in a hurry; by just writing a prescription without listening to patients’ problems or the details of sickness. But there is another doctor who, whenever they see him, patients become happy and comfortable. ‘Eeeh, our doctor has arrived, he has a good heart.’
Collectively, these accounts suggested that participants’ access to information about a doctor’s behavioural and technical reputation from their social networks and peers facilitated their initial trust judgement before physically encountering the doctor. This raises a question as to how encountering a doctor with an initial distrust judgement impacts what then transpires in a physical encounter.
Factors shaping patient trust in doctors during therapeutic encounters
When examining participants’ accounts of factors shaping doctors’ trustworthiness during therapeutic encounters, the authors heuristically categorised the encounter using four phases: rapport building, disease diagnosis, disease management and farewell. Participants described different aspects of doctors’ behavioural and technical competence that shaped their trustworthiness in each phase.
Rapport building: This phase marked the first few minutes of the patient–doctor encounter, and was characterised by a range of interpersonal activities that built a close and harmonious relationship in which both the patient and doctor understood each other’s feelings/ideas and communicated well. A doctor’s demeanour and communication that portrayed good customer care were valued by many participants as shaping their trustworthiness in this phase. Most participants characterised a trustworthy doctor as one who offered a warm welcome, exchanged greetings, appeared to be happy to see a patient, showed positive facial expressions (smiling) and sat in a good (respectful) posture when a patient entered the room. Furthermore, doctors who expressed gentleness, care/sympathy and good verbal communication (kind words and good language) were also considered trustworthy. In contrast, participants considered doctors who portrayed poor hospitality (eg bad language, verbal harassment, reprimands and harshness giving rise to fear among patients, showing no sympathy and being preoccupied with writing when a patient entered the office) as untrustworthy. Moreover, doctors who prematurely terminated the conversation, such as sending patients away by handing over a prescription without a conversation, were also regarded as untrustworthy.
Disease diagnosis: This phase was characterised by activities such as medical history taking, physical examination and ordering medical investigations to facilitate a correct diagnosis. In this phase, doctors’ perceived technical skills were valued by many participants as shaping their trustworthiness. When taking a medical history, more than half of participants characterised a trustworthy doctor as one who listened carefully, asked many (relevant) questions, engaged a patient in the discussion and took a detailed history. Participants further described doctors’ activities, such as inquiring about their general progress, and asking about other body systems or symptoms and medication use, as features of a trustworthy doctor. Mlasi (homemaker) said:
There are two kinds of doctors: the bad one, who when you meet, he doesn’t ask questions; and the good one, who asks a lot of questions ranging from your progress and how do you feel that day.
Conducting a physical (bodily) examination was another important technical skill that many participants reported as shaping their judgements of trustworthiness during this phase. Many patients characterised a trustworthy doctor as one who checked a patient’s blood pressure, listened to their chest or ‘heart’ (using a stethoscope) and touched where there was pain. Mabula (retired government officer) suggested that a bodily examination ‘comforts (the patient) psychologically’. Rose (nurse) affirmed that a physical examination makes a patient ‘trust a doctor’.
Explaining the findings of such examinations and medical investigations, and ensuring inter-session continuity, were also valued as shaping patients’ judgements of their doctors’ trustworthiness during this phase. More than half of the participants characterised a trustworthy doctor as one who discussed any findings/observations with them, ordered different and relevant medical investigations and explained the purpose of each. For example, Rose (nurse) considered the practice of ordering different investigations as making the patient feel like they ‘received appropriate and loving care’. Similarly, Magdalena (clinical officer) characterised a trustworthy doctor as one who ensured continuity of care by providing their location or contact details for future discussion of the results of medical investigations and disease management.
In contrast, demonstration of skills that could contribute to an incorrect diagnosis or patient dissatisfaction was described as shaping doctors’ untrustworthiness during this phase. Most patients characterised an untrustworthy doctor as one who portrayed poor listening skills, did not ask questions, wrote a prescription without a detailed history or was busy writing when the patient was explaining their medical concerns. An untrustworthy doctor was further characterised as one who rarely enquired about the patient’s progress from the last visit, rarely performed a physical examination and rarely ordered medical investigations. Rose (nurse) and Asha (farmer) suggested that an untrustworthy doctor always offered excuses for not ordering investigations or not performing a certain examination. Explanations such as ‘the BP (blood pressure) machine is not functioning’ were regarded as a ‘bad’ doctor’s excuse for not taking a patient’s blood pressure. Most importantly, encountering an untrustworthy doctor in this phase was described by most participants as contributing to poor outcomes such as an incorrect diagnosis, and unmet patient expectations, needs and desires, leading to uncertainty and dissatisfaction with care.
Disease management: This phase was characterised by doctors’ activities focused on disease management interventions. Similar to the diagnosis phase, doctors’ technical skills were valued by participants as factors that shaped their trustworthiness during this phase. Many participants characterised a trustworthy doctor as one who explained the implications of the results of medical investigations, engaged patients and negotiated treatment options, and offered appropriate medications for both primary and secondary diseases/symptoms. Similarly, a trustworthy doctor was characterised as one who adjusted the medication dosage, discussed any potential side effects and prioritised the patient’s welfare. In contrast, untrustworthy doctors were characterised as lacking the aforementioned skills and confidence in disease management. Some disagreement emerged regarding peer consultations among doctors, which was characterised by a doctor seeking a second opinion from their colleagues. While healthcare workers (eg Magdalena and Rose) regarded peer consultation as a doctors’ trustworthy effort to offer appropriate care, some non-healthcare worker participants regarded this as a sign of technical incompetence, which contributed to untrustworthiness.
Furthermore, descriptions of a trustworthy doctor as one who strove to maximise patient participation in treatment decisions were more commonly referenced by participants who were clinically trained. These participants (eg Magdalena and Rose) grouped doctors into two categories: those who were understanding (trustworthy doctors) and those who were not understanding (untrustworthy doctors). An understanding doctor was regarded as someone who acknowledged and promoted a patient’s right to participate in care and responded with ‘positivity when a patient questioned the treatment decisions’ (Rose, nurse). In contrast, a non-understanding doctor was described as denying a patient the opportunity to offer their insights when making treatment decisions. Magdalena (clinical officer) considered a non-understanding doctor as one that did not acknowledge a patient’s right to participate and would think that ‘[a patient is] instructing or teaching [them] what to do’ if treatment decisions were questioned. Untrustworthy doctors were also described as those who frequently affirmed their expert status (eg ‘I am the doctor’) to patients. This was described as occurring by either dictating the treatment decisions (as mentioned earlier) or questioning the logic behind a patient’s therapeutic actions and rejecting any treatment that other doctors had previously offered without justification. Neema (small business owner) recalled an encounter with a doctor who questioned her decision to use a ‘homemade remedy for symptom management’. In support, Nyazula (medical assistant) recalled an encounter with a ‘bad’ doctor whose actions contributed to her non-adherence to medications:
I went to see a doctor. Upon arrival, I told him that I am a known hypertensive patient and I am sick. He started asking furiously ‘why are you taking all these medications? They want to kill you entirely … all four antihypertensive?’ So, he crossed [cancelled] all the medications that I was using that time. It made me feel weird. So, I lost faith completely in that doctor. I didn’t even use the medications he prescribed.
Some non-healthcare worker participants considered patients’ participation in care a good thing, but affirmed having been denied such opportunity by doctors. Regina (farmer) had ‘never seen a doctor offer that opportunity to a patient’ and noted that a ‘bad’ doctor ‘often dictates everything in terms of advice, medication and a patient is expected to concur with it’. Budodi (homemaker) indicated that a ‘bad’ doctor ‘only tells [the patient] to go and use medications’ and return if they do not feel well.
Finally, some participants described referrals to other doctors or healthcare facilities as an indication of a doctor’s honesty in recognising the limits of their expertise when the decision was made at the right time. However, other participants suggested that when a referral was a consideration, a trustworthy doctor would negotiate with patients by explaining referral options. This was because non-negotiated referrals may result in blame upon facing unfavourable circumstances at the referral point. It is important to note that referrals may also occur as part of disease diagnosis.
Farewell: This phase was characterised by activities that marked the end of a physical encounter and parting. In this phase, a doctor’s behaviour, demeanour and communication were valued by participants as shaping their trustworthiness judgement. Compassion, offering hope, assurance of relief or healing, honesty and ensuring continuity with care were described as shaping doctors’ trustworthiness. Magdalena (clinical officer) suggested that a trustworthy doctor ‘would be honest when they could not manage a medical problem’.
Clarifying patients’ post-encounter obligations was also considered a feature of a trustworthy doctor. Some participants characterised a trustworthy doctor as one who insisted the patient should find, use and adhere to medications, and explained potential side-effects and what to do should they occur. Some participants considered a trustworthy doctor as one who negotiated with the patient on when to return for care. Others characterised a trustworthy doctor as one who was accessible to offer post-care remotely or visited a patient at home when a need arose. Additionally, most participants characterised a trustworthy doctor as one who wished the patient a quick recovery, thanked the patient for coming and welcomed them to come again for any problem when ending the encounter. Magdalena (clinical officer) said:
At the end of the services you say goodbye to each other. The patient would say ‘Okay, let me give you a chance to see other patients and have a nice work’, I would also say have a nice work/day as well. That is the kind of a doctor who makes you feel that you trust him.
Dishonesty, telling lies and failure to keep patient information confidential by sharing with non-clinical personnel or people outside medical care did not emerge as issues when participants were talking about doctors’ trustworthiness. However, such issues did emerge when talking of untrustworthiness.
Doctors’ trustworthiness after therapeutic encounters
Participants’ accounts indicated that, in addition to other factors, a perception of relief, healing or cure moved trust to the highest level or ‘complete trust’. A good example was offered by Rebeka (small business owner), who described ‘completely’ trusting a doctor who ‘… prescribed medications that brings relief after taking them’. In contrast, most participants characterised an untrustworthy doctor as one whose treatment interventions did not bring relief, healing or cure. The absence of relief, healing or cure was described as generating uncertainty and dissatisfaction, and perhaps leading to complete distrust. Misuka (nurse) said:
I went to a doctor, he gave me medications and I used them without a relief. Honestly, I wasn’t satisfied with the treatment. That is why I left that doctor and started looking for my [different] doctor. This is because I used medications for a long time. I used the first type without a relief and changed to the second type without a relief. That is when I decided to look for [a different doctor] because I came to believe that, the doctor who was treating me was unable to cure me.
Using subsequent visits as an opportunity to rectify any mistake that might have fuelled distrust in previous encounters was the most interesting finding from participants’ accounts of a trustworthy doctor. Masaza (teacher) described a stigmatising conversation with a doctor in the first encounter that led to distrust; however, she later developed trust after that doctor apologised in a subsequent visit. A doctor’s apology was described as not only offering comfort to the patient, but also setting the ground for cooperative choices to either resolve the error or work towards a more favourable outcome. In support, Mwasi (small business owner) described how a doctor’s apology shaped her trust judgement:
I came here for the first time and the doctor told me that I don’t have a problem, but then the same doctor diagnosed a problem after examining me when I came back. He personally felt sorry for me. He said to me ‘sorry for having endured this problem’. It made me very happy that the doctor could detect my problem. He kept saying ‘sorry … sorry … sorry’. To be honest, I was very comforted that day … I felt healed before even using the medications … and I trusted that doctor.
This indicated that an apology from a doctor when mistakes were made was among the most important factors shaping perceptions of trustworthiness.
Although doctors’ reputation, behaviour and technical skills were valued by participants as shaping patients’ trust judgements, some participants (both healthcare workers and non-healthcare workers) suggested that a patient’s own behaviours and institutional resources may also play a significant role in shaping trust in therapeutic relationships. However, this aspect was beyond the focus of the present article. Table 2 summarises participants’ descriptions of factors shaping doctors’ trustworthiness and untrustworthiness.
Table 2: Patients’ descriptions of factors shaping doctors’ trustworthiness and untrustworthiness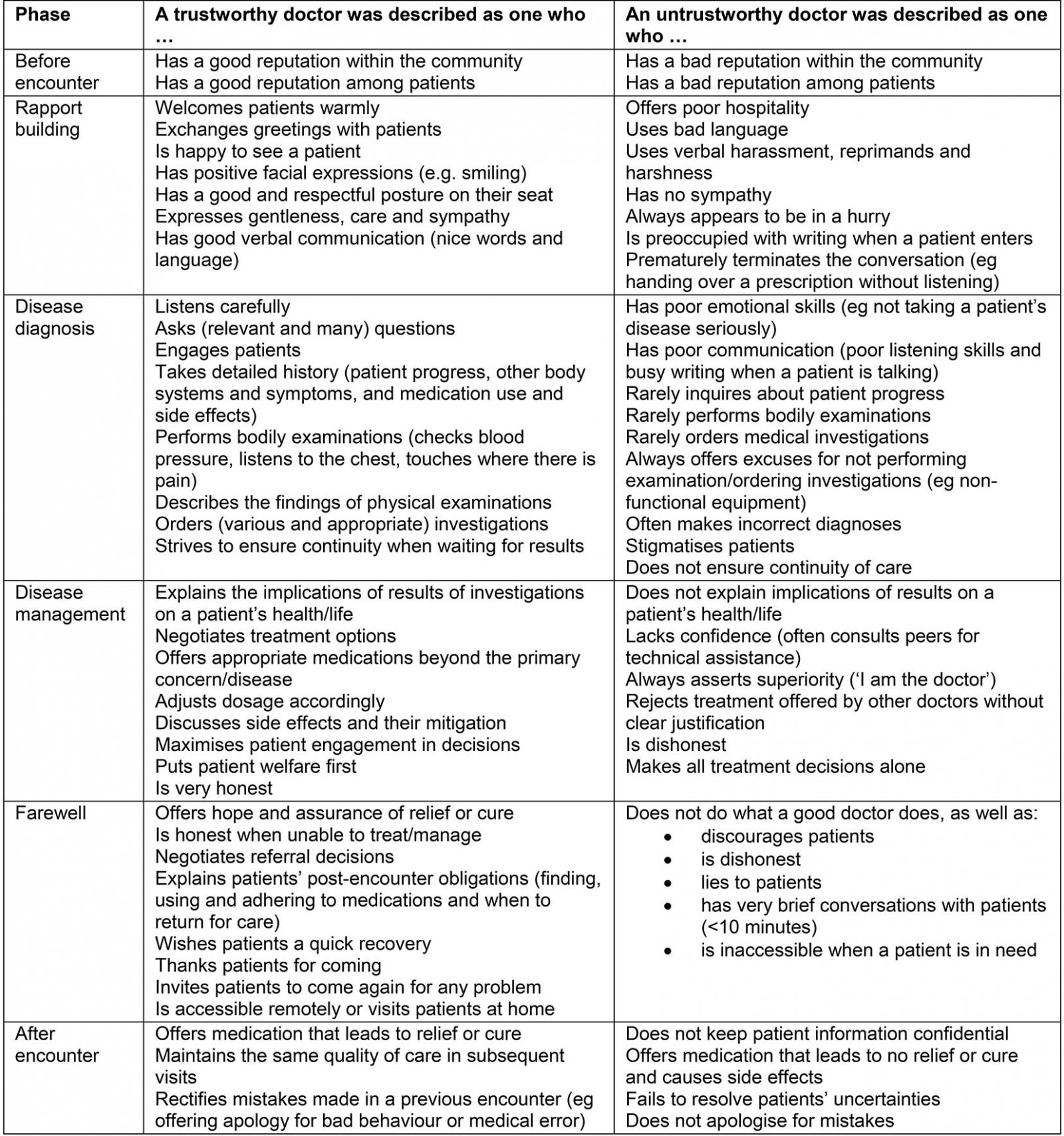
Discussion
This article explored patients’ perspectives of the behaviours and skills that shaped their judgement of doctors’ trustworthiness in rural Tanzania. It important to note this article is based on a broader qualitative inquiry that examined issues beyond factors shaping patient trust in doctors, and included what trust means and its perceived benefits38. An extensive review of both empirical and theoretical literature revealed that trust is multifaceted and can be contextualised. There is neither an overarching theory of interpersonal trust in the patient–doctor relationship or a universal framework that attends to all aspects of patient trust in doctors38. Therefore, this research was designed to investigate trust by considering its complexity and multifaceted nature in a specific context, as suggested by some social theories. This strategy allowed a contextualised account of patient trust in doctors in rural Tanzania to emerge throughout data collection and analysis, without viewing trust through an existing theoretical framework. However, the authors understand that investigating trust this way positioned the research within the constructivist paradigm39,40. This means that the research relied on participants’ descriptions to examine how patient trust in doctors was constructed in a specific context (rural Tanzania) as a construct shaped by different factors, rather than assuming it to be a positivist concept with a universal definition. The authors recommend that further studies on this topic consider using a theory-driven inquiry in a similar context. In an attempt to contextualise trust, the present findings draw on accounts of two distinct groups of participants: healthcare workers as patients (nurses, clinicians and attendants) and non-healthcare workers (farmers, teachers, homemakers, small business owners and retired government officials).
Patients’ judgements of doctors’ trustworthiness started with an initial level of trust before the therapeutic encounter, which was shaped by access to information about a doctor’s reputation from social networks (family, friends and neighbours) and other patients. The finding that a doctor’s reputation in society shaped initial trust appeared to be novel and has not been reported in previous empirical research. However, a similar concept can be seen in some theoretical literature41-43. For example, Lewicki et al41 and Conviser42 referred to this initial trust as ‘established trustworthiness’ and considered it as being based on a trustor’s judgement of a trustee’s abilities and rank compared with others using information accessed before a physical encounter. The concept of a doctor’s ‘abilities and rank among peers’ indicates their ‘technical reputation’ shapes initial patient trust. Furthermore, this finding suggested that, in rural Tanzania, a doctor’s reputation in patients’ social networks (family, friends and neighbours) and among other patients may be an important driver for patients’ initial trustworthiness judgements. This may contribute to patients’ decisions early in seeking healthcare from trustworthy doctors, and it further highlights the need to tap into the influence of family, friends, neighbours and other patients in seeking to improve patients’ initial trust in doctors.
During therapeutic encounters, a patient’s judgement of a doctor’s trustworthiness appeared to be shaped by the doctor’s actions. In this study, most participants cited actions related to a doctor’s behaviour and demeanour that demonstrated customer care, understanding and sympathy as important factors shaping trustworthiness. Other actions cited as important in participants’ judgements of doctors’ trustworthiness included technical skills related to history taking, physical examinations, correct diagnosis, treatment decisions and continuity of care. These findings were consistent with those of studies from high-income countries10-21. This implies that these factors need to be addressed more broadly when designing interventions to improve trust in doctors in low-income Africa. Some of the trust improvement interventions that address these factors in high-income countries may also be transferable to rural Tanzania and vice-versa.
In contrast to the findings of previous studies, the present study’s participants described a number of factors shaping doctors’ untrustworthiness. These factors mainly related to a doctor’s failure to demonstrate behaviour, demeanour and technical competence that shaped trustworthiness judgements among patients. Doctors’ bad behaviour, poor demeanour and perceived technical incompetence during therapeutic encounters emerged in participants’ descriptions as both shaping patients’ judgements of their untrustworthiness and fuelling patients’ uncertainty, fears and dissatisfaction with the care provided. This suggested that examining factors shaping doctors’ trustworthiness and untrustworthiness could offer more information for designing trust improvement strategies. For example, some participants described doctors’ untrustworthiness as the reason for poor adherence to medication and weak continued engagement with healthcare services. The factors shaping doctors’ untrustworthiness and contributing to patients’ dissatisfaction with care, non-adherence to medical interventions and weak continued engagement with healthcare in the present study were consistent with those described in previous studies on patient–provider relationships in general care, maternal and child health care and HIV care in low-income Africa44-48. This suggests that the negative impact of doctors’ untrustworthiness in low-income Africa, as described by patients receiving hypertension care in rural Tanzania, extends beyond care for non-communicable diseases to other health conditions. In other words, perceptions of untrustworthy doctors held by patients seeking hypertension care are likely to be similar to the perceptions of patients seeking care for a range of other medical conditions. This is particularly important because doctors offering hypertensive care in rural Tanzania also offer medical care for other acute and chronic conditions.
It is important to acknowledge that there may be some confusion regarding the characterisation of technical skills and rapport-building factors that emerged as shaping trust in this rural Tanzanian context. The present findings characterised skills such as doctors’ use of medically grounded technical expertise to explore signs and symptoms through listening carefully to patient complaints, asking many questions relevant to the complaint/disease, engaging patients in discussion about signs and symptoms and taking a detailed medical history as technical competences that shaped patient trust. This finding was consistent with a previous study that indicated most trust research in healthcare identified patients’ perceptions of provider competence/skills shaping trust as those related to ‘knowledge, expertise and ability to diagnose and treat, quality of care, understanding of/interest in patients’ problems, thoroughness, willingness to share correct information and treatment success’38 (p. 53). These technical skills differ from rapport-related activities that focus on building ‘a close and harmonious relationship in which patients and doctors understand each other’s feelings or ideas and communicate well’ at the beginning of the encounter. Rapport-related activities are those shaping patient trust, such as the doctor’s demeanour and communication, that portrayed good customer care (eg a warm welcome, exchanging greetings, appearing happy to see a patient, smiling, sitting in a respectful posture when a patient entered the room, gentleness, care/sympathy, and good verbal communication). However, it should be acknowledged that some of the skills identified as ‘technical’ in this study may fall under ‘rapport building’ in other studies and vice-versa. This suggests that, regardless of the blunted distinction, interventions to improve patient trust in doctors in the rural Tanzanian context need to consider both technical and rapport-building skills.
Although doctors’ good behaviour, demeanour and perceived technical competence emerged as central to patients’ judgements of their trustworthiness in rural Tanzania, this does not underscore the need for ‘trustworthy patients’ in therapeutic relationships. Some trust literature has proposed that a patient’s own behaviour and biography may influence a doctor’s reciprocity during therapeutic encounters3,10,12,15,49,50. This implies that efforts to promote doctors’ trustworthiness also need to encompass those seeking to construct trustworthy behaviours among patients.
It is also important to acknowledge that doctors’ trustworthiness may be shaped by the trustworthiness of the institutions in which they work. Some studies have indicated the availability of resources (eg sufficient doctors, medicines and medical equipment) as essential in creating an environment where trust can be established and sustained3,49,51. The need for physical examinations and medical investigations as described by participants in the present study may not be fulfilled in the absence of functional medical equipment and medical supplies. Although these issues are beyond the scope of this article, a doctor’s ability to negotiate for alternatives to institutional barriers remains an important skill that may shape patients’ judgement of their trustworthiness. These issues also suggest that trust improvement interventions in rural low-income Africa need to extend beyond patient–doctor relationships to consider health system barriers that contribute to patient distrust in doctors in Western practice. However, given the limited research on patient trust in doctors in rural low-income Africa, further research is needed to generate evidence on how institutional resources and a patient’s own history impact their trust judgements of doctors in this setting. In addition, more research is needed on how trust changes over time during and after therapeutic encounters and its measures in the study setting, given the long-term therapeutic nature of hypertension/non-communicable disease care.
Limitations
This article did not explore all features pertaining to doctors that shape patients’ perception of their trustworthiness, such as factors that are beyond the doctors’ behaviour, demeanour and perceived technical competence (eg age, tribe and gender). Most participants identified as being of the Sukuma tribe, and the interviews were conducted in Swahili. These patients were selected from characteristically rural districts (over 95% rural occupancy) characterised by public monopoly in health services52, centralised hypertension care, prolonged waiting times, low use of health services and medical pluralism37,53-56. Similarly, the accounts of women participants (n=28) used in this manuscript exceeded those of male participants (n=6). As noted elsewhere38, possible explanations for this include that 9 out of 12 enrolment assistants were female, making it more likely to enrol women; the study was conducted during a farming season, meaning men may have prioritised farming activities over study participation; and hypertension is more prevalent among females than males in Tanzania, possibly making women more likely to frequently seek hypertension care compared with men. Therefore, the present findings cannot be applied to patients and doctors from both sexes, and those from culturally, linguistically and structurally diverse backgrounds. Only considering patients’ accounts in this article may be taking the path of previous studies that have restricted the examination of factors shaping trust to patients’ perceptions. However, the present study included healthcare workers (eg nurses, medical attendants and clinicians) who participated as patients, and these participants often drew on their experiences as agents of healthcare institutions. This facilitated bringing providers’ voices to this inquiry. Additionally, all interviews were conducted by one author (KI) who has a medical background and has previously worked as healthcare service advocate in Tanzania. This might have impacted the interview process, choice of themes, related subthemes and codes that were considered most appropriate. It might also have affected the interpretations of participants’ accounts and the conclusions in seeking to answer the research questions. However, peer consultation within the research team was used throughout this study to help address these issues.
Finally, the unit of analysis employed in this study was a medical consultation rather than the longitudinal patient–doctor relationship. The authors’ choice to analyse the patient–doctor relationship in the context of a consultation was dictated by what defines the relationship itself – a physical encounter during medical consultation – particularly in low-income rural settings where non-physical patient–doctor relationships are largely unavailable. In addition, factors shaping patient–provider relationships beyond the experiences surrounding a medical consultation were examined. For example, developing initial trust without an individual patient’s experience of medical consultation, and trust based on treatment outcomes where the ability of a doctor’s treatment to bring relief and cure, emerged as shaping trust. As this was the first study to be conducted in this rural context, further studies may look at the patient–doctor relationship from different perspectives.
Conclusion
Improved patient trust in doctors is documented to impact patients’ service uptake, adherence and continuity with care1-9. The practical implications of the study findings include three major premises. First, the findings provide a gateway for trust improvement interventions by identifying specific factors shaping doctors’ trustworthiness or untrustworthiness that need to be promoted (or discouraged) to improve patient uptake, adherence and continuity of primary healthcare services. Participants’ accounts of the factors that shaped doctors’ trustworthiness in rural Tanzania indicate a need to engage both patients and doctors as partners in health care, as well as addressing structural barriers at the institutional level to maximise the success of trust improvement interventions. Second, the findings of this study provide doctors with evidence of aspects that can be used to self-audit their current practices versus those desired by their patients to improve trust. Third, this study generated a list of doctors’ behaviours, demeanours and technical skills that may be useful in improving medical training curricula to foster a culture of trustworthiness among medical graduates in rural low-income Africa settings.
Acknowledgements
The authors thank Professor Heather Worth and Professor Alex Broom of the University of New South Wales, Australia for their input into conceptualisation, design and data gathering; Dr Ntuli Kapologwe, the former Region Medical Officer of Shinyanga, for support during data gathering in Tanzania; and Audrey Holmes and the Aga Khan University School of Nursing and Midwifery (East Africa) for proofreading support.
References
You might also be interested in:
2012 - 'It's a regional thing': financial impact of renal transplantation on live donors


