Introduction
A focus on primary health care remains fundamental to the overall performance of the health system, providing better health outcomes, improved equity and better cost efficiency1. Shortages and maldistribution of the GP workforce2,3, and the subsequent impacts on healthcare access and delivery, are longstanding concerns in Australia primary health care4. By 2030, it is projected that the Australian GP workforce will be increasingly unable to meet growing demand for services5. The retention of GPs within the workforce is a national issue, with GPs in Australia indicating an intention for earlier retirement and fewer than half (48%) of current GPs intending to still be practising in 10 years time6.
The impacts of the emerging GP workforce deficit and maldistribution of GPs in Australia are manifested in individual general practices and in the communities they service. Attraction to, and retention in, these practices is a major issue. Attraction to a practice has been the subject of much attention7-9, but retention has been less well explored10,11 and is being increasingly recognised as just as important as recruitment strategies. It has been demonstrated in Australia and internationally that GP trainees with rural backgrounds or rural experience during undergraduate or postgraduate medical training are more likely to practise in rural areas9,12. While remuneration, workload and location-related issues of lifestyle, spousal employment, and child education are factors in retention (as well as in attraction), characteristics of practice work tasks may plausibly have a role. These may be more relevant to retention than to attraction. Being able to provide comprehensive, holistic primary care, including out-of-practice services, may be an attractive feature of a practice. This would be in keeping with the aims of primary care including the provision of comprehensive long-term, person-focused care1.
A broader review of some other reasons why GPs gain satisfaction from their work will be informative. GPs appreciate developing strong and rewarding interpersonal doctor–patient relationships and caring for several generations of the same family13,14. A particular aspect of ongoing interpersonal care, and an intrinsically rewarding area of GP work, is the out-of-practice home or nursing home visit. The home visit has long been regarded as core to general practice15. GPs undertake home visits for a range of reasons. Visits may be reactive to a sudden deterioration in a patient’s health. They may also be proactive, especially for patients who, due to chronic disease, palliation or debility, are unable to travel, and involve the development of relational continuity of care between GPs and their patients16. A survey of GPs in Australia17 found approximately 64% of respondents indicated they do undertake such visits.
A singular aspect of GP workforce and retention at the individual practice level is retention of registrars (vocational trainees in general practice) who have completed part of their training in the index practice. A major factor in many teaching practices taking on a training role is workforce. Registrars constitute 14.7% of the Australian GP workforce by headcount18, with an increase in proportion from 2015 to 201919. Registrars also make up a higher proportion of the GP workforce in regional and rural areas, with 23.0% of Modified Monash (MM) 2 areas, 22.5% in MM 3 areas and 22.7% in MM 4 areas19,20. Recent graduates from general practice training also make up a sizable portion of the GP workforce. Hence, registrars rotating through practices (for training terms for 6 or 12 months) are vital to many practices’ short- to medium-term viability. There is also the longer term viability consideration, for training practices and the communities they serve, of the potential recruitment of registrars who have trained in these practices to remain employed at these same practices longer term post-Fellowship. Thus, participation in the GP vocational training program, and retention of registrars post-Fellowship, is a potentially valuable issue for practices, especially in areas of workforce shortage. Rural and remote GP practices are disproportionately affected by the growing GP workforce shortage, with additional compounding issues of professional isolation, uncompetitive remuneration and viability challenges21. Even in areas without workforce shortage, post-Fellowship retention of former registrars may have practice quality implications, enabling employment of ex-registrars who have demonstrated aptitude in that practice.
We aimed to establish the prevalence and associations of retention of general practice registrars in the same practice, that is, working as an established GP specialist in a practice in which they trained.
Methods
This analysis was a component of the New alumni Experiences of Training and independent Unsupervised Practice (NEXT-UP) study. The detailed study protocol is presented elsewhere22. Briefly, NEXT-UP was a questionnaire-based cross-sectional study of early-career GPs, augmented with data contemporaneously recorded as part of the participants’ general practice vocational training program.
The participants were former registrars (‘alumni’) of three regional training organisations that deliver general practice training across New South Wales, Tasmania, the Australian Capital Territory, and eastern Victoria (in total, 43% of all Australian general practice registrars)23. At the time of the questionnaire survey, participating alumni were within 6 months to 2 years post-completion of vocational training (having attained Fellowship of the Australian College of General Practitioners or the Royal Australian College of Rural and Remote Medicine between January 2016 and July 2018, inclusive).
Recruitment and questionnaire
Eligible alumni were both emailed and mailed invitations to participate, along with the study questionnaire. The questionnaire elicited information regarding the alumnus’ current practice and their training experiences. If the alumnus consented, questionnaire data were subsequently linked to the alumnus’ routinely collected vocational training data.
Outcome factor
The outcome of interest in this analysis from NEXT-UP was whether the registrar had previously worked at their current practice during vocational training.
Independent variables
Independent variables in regression analyses were age, gender, rurality of current practice, socioeconomic area of current practice, Australian / International medical graduate (AMG/IMG), current full-time/ part-time status, provision of home visits / nursing home visits / after-hours care, provision of undergraduate teaching or registrar supervision, Fellowship year, spousal status and employment, provision of other regular medical work, full-time / part-time status during training, number of different practices worked in during training, rurality of training (using the MMM as a dichotomous outcome (MM 1 v MM 2–7 (with the latter described in this article as regional–rural areas)20 and socioeconomic status of training area (deciles of the Socioeconomic Index for Area – Index of Relative Social Disadvantage (SEIFA-IRSD)24, examination performance in college-level exams.
Statistical analyses
Descriptive statistics included frequencies for categorical variables and mean with standard deviation (SD) for continuous variables.
Logistic regression was used to establish associations of the alumni currently working at their former training practices. Univariable analyses were conducted on each covariate, with the outcome. Covariates with a univariable p-value less than 0.20 were considered for inclusion in the multiple regression model. Once the model with all significant covariates was fitted, model reduction was assessed. Covariates that were no longer significant (at p<0.2) in the multivariable model were tested for removal from the model. If the covariate’s removal did not substantively change the resulting model, the covariate was removed from the final model. A substantive change to the model was defined as any covariate in the model having a change in the effect size (odds ratio) of greater than 10%.
Diagnostic tests were conducted to assess goodness of fit, using the Hosmer–Lemeshow test for logistic models.
The regression modelled the log odds that a registrar had previously worked in the current training practice. Significance was declared at the conventional 0.05 level, with the magnitude and precision of effect estimates also used to interpret results.
Analyses were programmed using STATA v14.2 (StataCorp https://www.stata.com) and SAS v9.4 (SAS Institute; https://www.sas.com/en_au/home.html).
Ethics approval
The NEXT-UP study has approval from the University of Newcastle Human Research Ethics Committee (approval H-2018-0333). All participants provided informed consent to participate in the research.
Results
There were 354 respondents (response rate 28%), of whom 337 were currently working clinically in general practice. Of these, 322 provided data regarding previous training practice retention, with 59% (95% confidence interval (CI) 54–64%; n=190) having previously worked at their current practice as registrars. Within the sample for which data were available, among respondents who reported currently working in a regional–rural practice location (n=100) (28% of total respondents), 69% (95%CI 59–77%) reported having previously worked at their current practice during training. For participants who reported currently working in a metropolitan (MM 1) location (n=219), 55% (95%CI 48–61%) reported working previously at their practice during training.
The characteristics of participating alumni and their current practices are presented in Table 1.
Characteristics associated with registrars having previously worked at their current practice during training are presented in Table 2. Results of multivariable logistic regression are presented in Table 3. Goodness of fit tests showed the model was a good fit.
On multivariable analysis, GPs were more likely to be working in a practice in which they had trained if the practice was located in an area of a lower socioeconomic status (adjusted odds ratio (aOR) 0.82 (95%CI 0.73–0.91), p<0.001 for each decile of the SEIFA-IRSD) and if the practice provided two or more of home visits, nursing home visits or after-hours care services (aOR 4.29 (95%CI 2.10–8.75), p<0.001). Registrars were less likely to be retained by a practice if the training was completed in a regional–rural area (aOR 0.35 (95%CI 0.17–0.72), p=0.004).
On univariable analysis, practice retention was greater for AMGs compared to IMGs (OR 3.28 (95%CI 1.91–5.64), p<0.001), with some evidence for an association on multivariable analysis (OR 2.06 (95%CI 0.86–4.94), p=0.11). There was a similar relationship for part-time (compared to full-time) alumni (OR 1.80 (1.11–2.92), p=0.017 on univariable analysis; and OR 1.70 (95%CI 0.90–3.21), p=0.10 on multivariable analysis). And for region 2 (compared to region 1): (OR 1.95 (95%CI 1.12–3.40), p=0.018 on univariable analysis; and OR 1.80 (95%CI 0.92–3.45), p=0.089 on multivariable analysis).
Table 1: Participant characteristics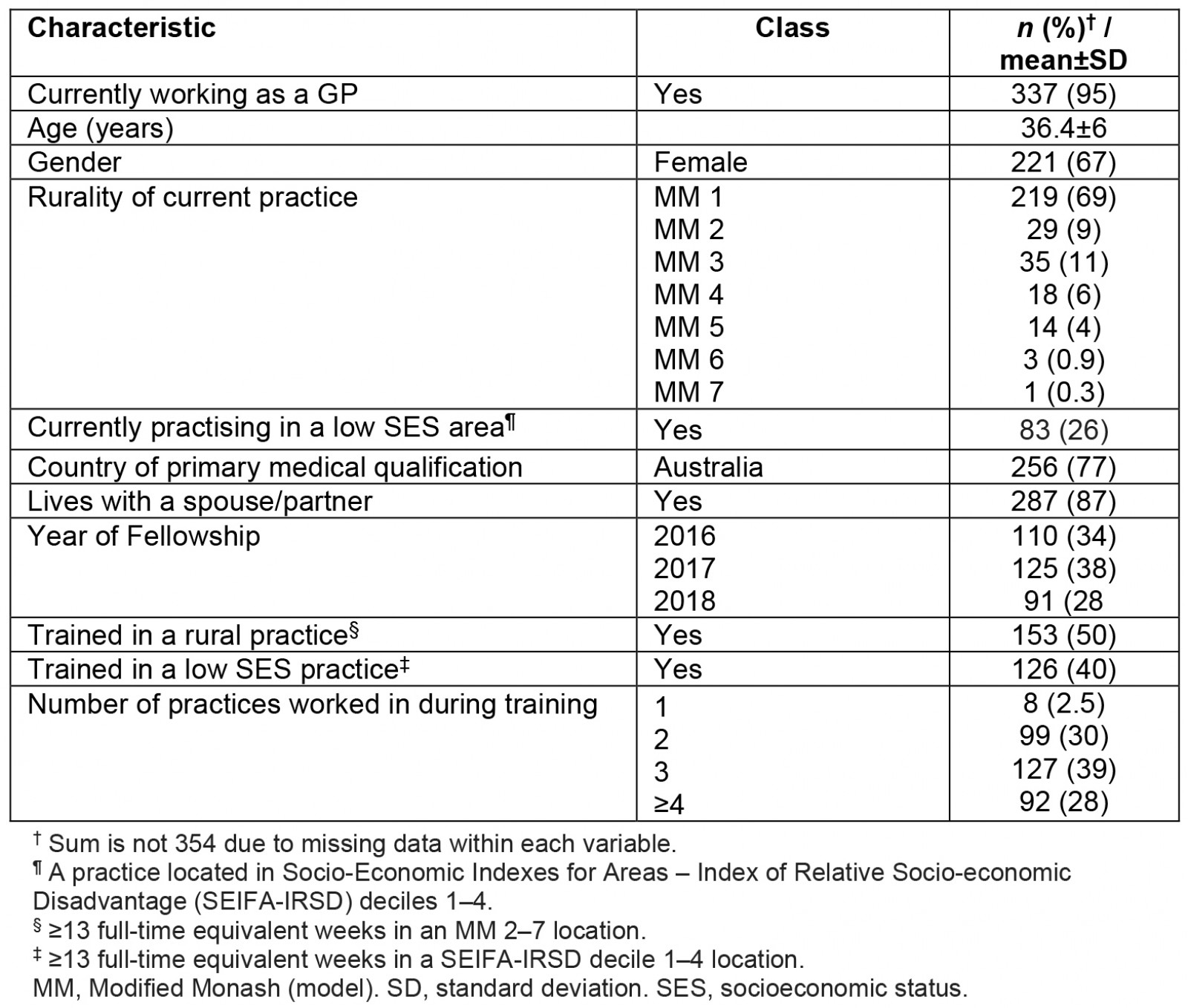
Table 2: Characteristics associated with alumni having previously worked at their current practice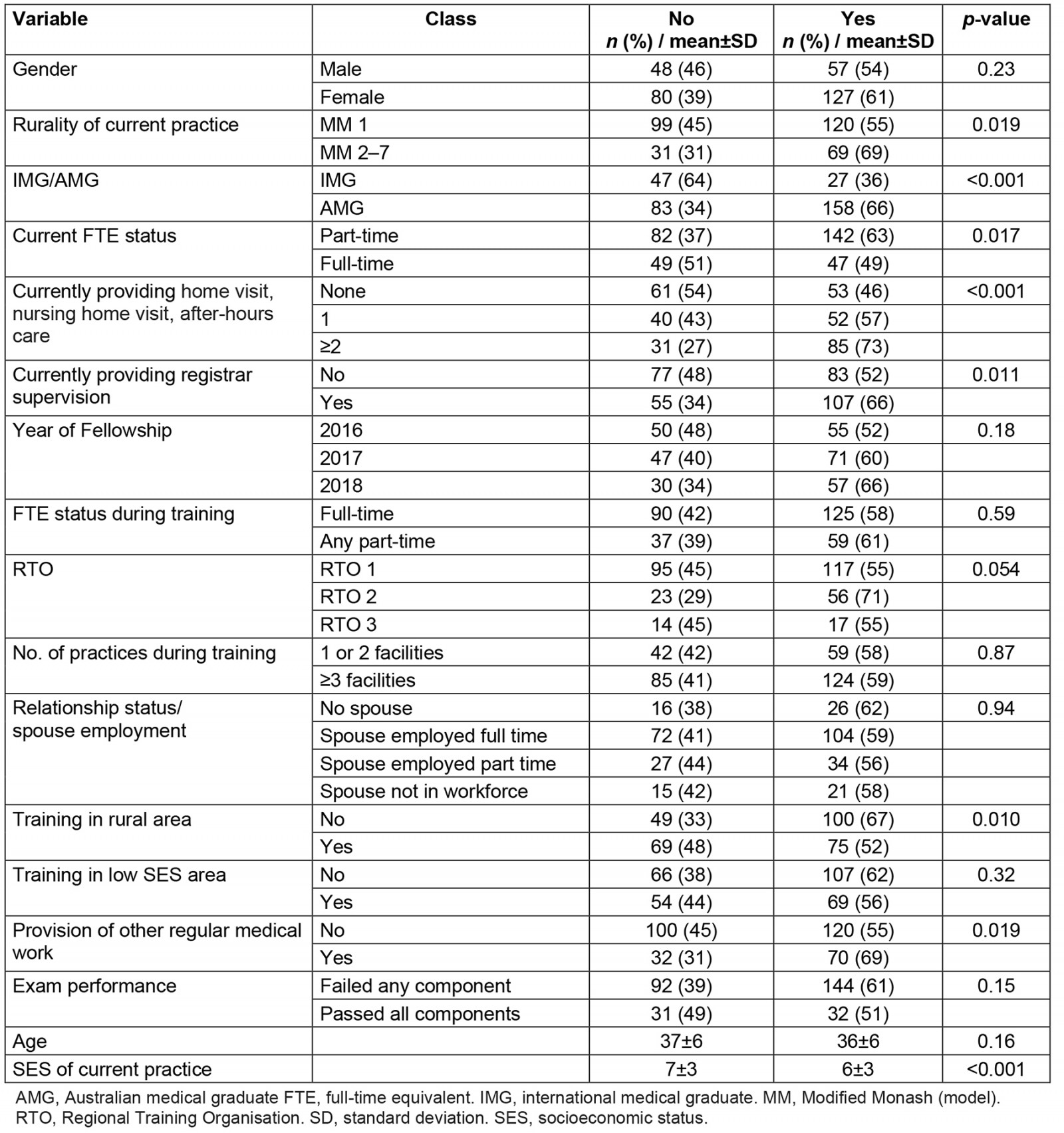
Table 3: Univariable and multivariable regression models with outcome ‘currently practising in a practice in which the alumni had worked as a registrar during GP vocational training’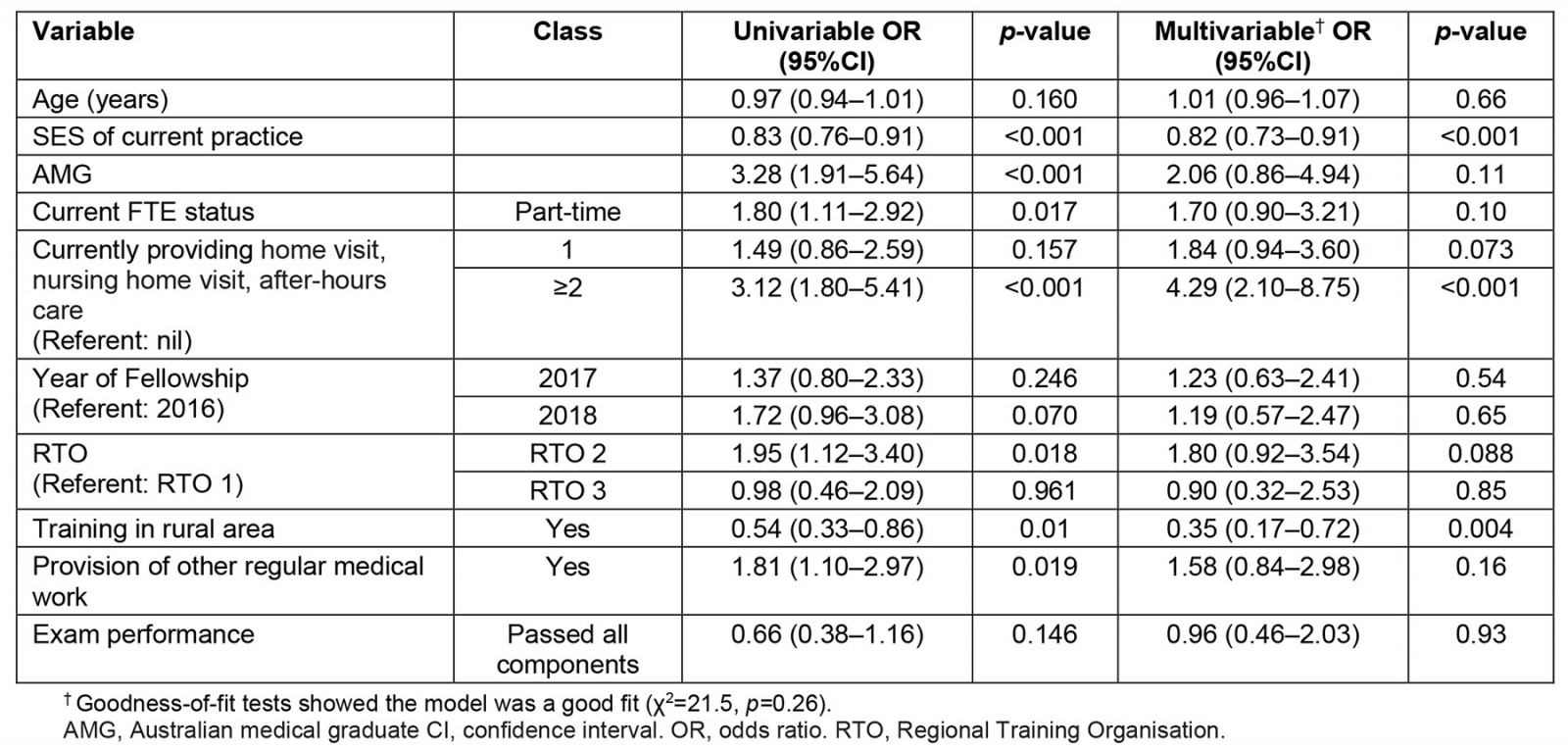
Discussion
This study demonstrated that GPs were more likely to be retained by and working, as established specialist GPs, in a practice they had trained in, if the practice was located in a lower socioeconomic status area, and if home visits, nursing home visits or after-hours care services were provided. They were less likely to remain in a practice if their training was completed in a regional–rural area.
There was some evidence that Australian medical graduates and those working part-time were more likely to be retained in training practices.
‘Retreat’ from rural areas
We found that a regional–rural training location was associated with markedly reduced odds of currently working in a practice in which the GP had trained. This is not unexpected given the existing literature on Australian GP practice location25.
Though training placement policies result in a sizable proportion of regional, rural and remote GPs being trainees, most of these GPs do not continue to practise rurally, and the proportion of GPs practising rurally declines by seniority of career stage (from late career to mid-career to early/establishing career)26. There is even an apparent ‘flight from rural areas’ commencing during training, with term 2 and term 3 registrars being considerably less likely to work rurally than term 1 registrars27. Thus, despite significant government investment in expansion of general practice training in regional and rural areas, the numbers working in rural and remote communities have not kept pace with the increase in medical graduates28. This remains the case despite regional–rural areas being identified as interesting and rich learning environments27,29. The exact reasons behind the retreat of trainees from these areas once they attain Fellowship remain unclear but working in regional–rural practice does entail greater challenges and stresses for registrars including greater workload and responsibility30, risk of burnout31 and perceived higher risk of occupational violence32. Furthermore, Australia is one of many developed countries to rely on international medical graduates (IMGs) to fill positions in ‘areas of need’33. IMGs practising in Australia benefit from government policies that facilitate their immigration to Australia by working in communities with workforce shortage under the 10-year moratorium34. They represent up to 40% of the Australian GP workforce in these areas35. This ‘enforced’ separation from social supports and lack of other factors encouraging ongoing work in these communities such as opportunities for professional development, being a part of the community, work satisfaction and cultural considerations means many GPs and IMGs relocate to urban areas upon completion of their mandated requirements25.
Out-of-practice care and retention in regional–rural practices
The strongest association with GP retention at a practice found in this study was practice provision of home visits, nursing home visits and after-hours care as part of its services. This is a counterintuitive finding, made in the context of these activities being demanding, and time- and remuneration-inefficient17,36,37 and of there being a global decline in the number of this type of visit being done by GPs, including those in rural areas38. This trend is occurring in the context of the primary target group for these visits, older people with multiple morbidities, growing in number36,39. Evidently there are other professional and educational motivators for providing care in an out-of-practice and after-hours setting.
Previous research has demonstrated that the rates of out-of-practice and after-hours care provision by GPs are greater in rural and regional areas than in metropolitan areas40,41 and in areas of socioeconomic disadvantage42. Our study implies that there is increased desirability for working in practices that do provide these services and that the higher rates of trainee retention seen in these practices should benefit rural and regional practices. The existing literature also suggests rural practices are good learning environments for trainees27,43-45.
It may well be that there is an altruistic reason for GPs to engage with out-of-practice care. GPs know their patients’ medical histories, can undertake preventive care, manage chronic health conditions and coordinate their patients’ multidisciplinary care needs46. Previous research has demonstrated that GPs who do home visits during registrar training were five times more likely to still be doing this post-graduation, and those doing nursing home visits up to 11 times more likely to still be doing this post-graduation47. Furthermore, burnout levels were low and perceived achievement levels high among doctors involved in after-hours house calls in Australia48. Home visits provide an opportunity to learn more about the patient, observe their socioeconomic situation, the effects of interventions, and also to learn about oneself and the doctor–patient dynamic49, and this could be a humbling experience for trainees50,51. For many GPs, ‘it is not all about the money’52, though increased financial incentives for practising in rural regions did appear to have an impact on GP trainees being retained in rural areas53.
Critically, however, the capacity of provision of after-hours and out-of-practice care to retain trainees in regional–rural practices is outweighed by rurality overall being a major factor for trainees to move back to metropolitan areas. Unfortunately, our findings only reinforce the known poor retention of trainees in regional–rural areas, despite practices, training programs and rural experiences being generally positive for GP trainees30. While there is an overall movement of GPs towards metropolitan areas25,33,54, GPs working in regional and rural areas do tend to be more mobile than urban GPs and work in different practices, while remaining in rural and regional areas55. The findings of our study need to be interpreted in this context: though trainees may leave a practice, despite there being provision of a good learning environment and participation in out-of-practice and after-hours care, this does not necessarily mean that these trainees have left rural and regional areas. Rural practices should not be dissuaded from continuing to provide after-hours and out-of-practice care experiences as incentives for retaining registrars in their practices.
Socioeconomic status
It has been previously demonstrated that GP trainees working in areas of socioeconomic disadvantage were more likely to be full-time trainees, at the beginning of their training and have increased continuity of care with patients56. It was posited that areas of socioeconomic disadvantage provide greater learning opportunities for GP trainees56. The findings of this study support the attractiveness of this training environment and its capacity to retain general practice registrars, by showing that, for every decile increase in socioeconomic status, there is less likelihood that GPs were retained in these practices. It may be that there is greater professional and personal satisfaction for GPs working in these areas, even though it is less likely that other factors such as higher remuneration and ‘prestige’ are present. Satisfaction may be derived from fulfilling the social imperative of a GP in providing comprehensive, first contact, holistic, person-focused care over time1.
Implications for practice and policy
We have demonstrated that regional–rural training is negatively associated with GP retention within a training practice. This is despite provision of nursing home visits, home visits and after-hours care by the practice being strongly associated with retention (and these services during training having previously been demonstrated in the same GP population to be strongly associated with regional–rural training)27. There is declining interest in out-of-practice care among younger GPs15, with calls to remove this ‘anachronistic’ practice due to there being little evidence supporting the benefit to patients and GPs16. Our findings demonstrate that general practice registrars are finding professional value in the opportunity to participate in out-of-practice and after-hours care and there is a compelling argument to have these opportunities maintained as an essential experience of GP care.
The implication is that provision of these services by a practice attenuates to some extent the negative effects of regional–rural location on retention. A conclusion is that regional–rural practices should encourage and support their registrars to participate fully in provision of these services. This would add to the positive team environment and ethical practice desired by general practice registrars57. Somewhat more speculatively, given our interpretation that the mechanism of the services-retention association is via ‘holistic’ practice, other aspects of comprehensive care and continuity of care could be encouraged and supported in registrars’ experience.
Further qualitative research methods could elucidate and clarify the facilitators and barriers for registrars training in regional and rural areas from continuing to work in these areas.
From 2023, training provision and coordination transitioned to the Royal Australian College of General Practitioners and the Australian College of Rural and Remote Medicine. Within this model, the expansion of the rural generalist program may influence registrars to remain in their training practices. The rural generalist pathway aims to address geographical and vocational maldistribution58, developing a better-distributed rural medical workforce, by providing a rural base and training position with secure funding59. It is possible that the opportunity for GP trainees to have personalised matching of their career aspirations to training placements and practices would likely result in those practices being attractive options for post-fellowship retention.
Strengths and limitations
The response rate, while reasonable for a survey of GPs, is only modest60. This must be considered in assessing the generalisability of the findings. The characteristics of the study sample are consistent with those of Australian general practice registrars61. The multivariable analyses exploring associations in practice retention are post-hoc analyses and should be considered exploratory, with further research and replication indicated22.
The results of this study are derived from a previous system of training in Australia, which utilised regional training organisations. It is not expected that the findings from this study will be impacted by the change in training provision and coordination to a college-led model.
Conclusion
The findings from this study reiterate the known issue of general practice registrars leaving rural and regional training practices to work as established GP specialists elsewhere. A factor that encouraged retention was the provision of out-of-practice and after-hours care, services which are already performed more frequently in rural and regional areas. Despite the financial disincentive, a sense of obligation towards, and professional satisfaction derived from, undertaking out-of-practice care (which often encompasses patients with higher medical and social complexity) may underpin this finding. A fulfilment of the social imperative and duty of care to patients is achieved with out-of-practice care and adds to the attractiveness of a practice as a place of ongoing employment. Though the rurality of a practice cannot be changed, provision of home visits, nursing home visits and after-hours care services and providing a good working environment, with adequate educational and experiential opportunities, may help attract and retain general practice registrars that fit the ethos of the practice in terms of social conscience and temperament62 and hopefully continue to contribute to the rural GP workforce.
Funding
This research project is supported by the Royal Australian College of General Practitioners with funding from the Australian Government under the Australian General Practice Training Program, grant number ERG020.
Conflicts of interest
KF and MB were employees of General Practice Training Tasmania at the time of the study. AF, DM, ATa, AD and PM were employees of GP Synergy. CK and NS were employees of Eastern Victoria General Practice Training.
Data availability
The data that support this study cannot be shared for ethical and privacy reasons.
References
You might also be interested in:
2020 - Development of a referral pathway framework for fetal alcohol spectrum disorder in the Pilbara

