Introduction
Nearly half of the world’s population live in rural areas, and an estimated two billion people living in these areas do not have adequate access to essential health services1. Geographical barriers, lack of transport, increased distances and consequent increased cost of accessing healthcare services leads to poorer health outcomes for rural dwellers as compared to people living in urban areas1. A further critical factor underlying this inequality is a global lack of trained healthcare workers, which affects rural areas disproportionately1,2. Geographic and economic barriers, coupled with low healthcare worker density, lead to missed opportunities to provide timely patient care, in addition to inefficiencies and delays in care, with rural healthcare workers and patients wasting considerable time in transit3.
Approximately one in three people living in Ireland live in rural areas4. Rural communities in Ireland tend to have a higher proportion of elderly members, who have more healthcare needs. Thus, older rural dwellers face more transport challenges than their urban counterparts, which may hinder their access to healthcare settings5. Rural populations are also dwindling in many areas, with younger people moving to cities and towns for further education and employment opportunities. Thus, rural populations are both contracting and getting older, which gives rise to unique challenges that may not be apparent from simple calculations around supply of healthcare worker per head of population in a region.
In Ireland, mortality rates and hospital admissions are higher in rural areas6, and mortality rates are higher among children living in rural Northern Ireland7.
General practice plays a vital role in delivering improved community health outcomes, particularly in rural communities8. From a study from the US, adding primary care physicians to a region was more effective in reducing disease and death than adding equivalent numbers of secondary care clinicians9. Long-term continuity with primary healthcare services is associated with reduced all-cause mortality rates10-12 and it is widely recognised that money spent in primary care leads to considerable savings downstream for a population13.
Primary care clinic closures bring negative impacts on the populations they serve. Studies have shown that patients affected by a practice closure show a 12% decrease in annual GP visits and an 11% increase in specialist care usage14. Other research from the US noted that rural hospital closures have been shown to increase mortality rates from myocardial infarction, chronic obstructive pulmonary disease and stroke; whereas urban hospital closures had no measurable impact15.
Research by the Irish Department of Health estimates that by 2031 there will be a 46% expected increase in demand for primary care services across Ireland16, largely due to the ageing of our relatively young population (average age 38.8 years17 as compared to the EU average of 44.4 years18). While the total number of Irish GPs per 100 000 has been steadily increasing over the past 30 years, the number of rural Irish GPs has decreased over the past two decades4. Additionally, there is considerable geographic variation in the number of GPs and their workloads in rural Ireland19. Previous research in Ireland has shown that 89% of urban populations live within walking distance to the nearest GP clinic, compared to only 7% of rural populations20,21.
The purpose of this study is to explore the distribution of GP clinics among rural and urban populations in the Mid-West of Ireland. In addition, we investigate the impact on new travel distances if GP clinics were individually closed across the region.
Methods
Geography and rurality
Two counties in the Republic of Ireland were included in the study: County Clare and County Limerick. Both counties map onto the Community Healthcare Organisation 3 and are largely representative of the Republic of Ireland, with a mixture of urban and rural centres22. These two neighbouring counties have a combined population of 313 000 within an area of 6200 km2, although the density varies greatly across urban and rural subpopulations. The study area contains the third largest urban area in the country: Limerick City (population 94 000). Given Limerick City represents close to a third of the overall population in this area, it is from here on discussed separately to County Limerick. The analysis here presented is carried out at the Small Areas (SAs) level. SAs are the lowest level of official geography in Ireland and typically contain 80 to 120 dwellings. SAs were indexed into six categories of rurality per county based on the Irish Central Statistics Office classification for urban and rural areas4 (Table 1).
GP clinic identification
GP clinic locations in the area under study were identified using the Health Service Executive service finder website23. Individuals can access this database to determine the availability and location of health services in Ireland. While only County Clare and County Limerick SAs were investigated, GP clinics close to the border of this region were also located and analysed as it is not unlikely for a patient to cross a county boundary for GP care.
Distance calculations and clinic closure analyses
The open source statistical software R v4.2 in R studio (2022.07) (R Project; https://www.r-project.org) was used to map shapefiles that define SA boundaries in the Republic of Ireland and for subsequent analyses24,25. First, the XY centroid coordinates (latitude and longitude) of each SA was calculated using R’s SF package. Next, we calculated the distance from the centroid of each SA to its nearest clinic, in addition to the distance to the second nearest clinic. Finally, we calculated the difference between the first and second closest clinics (Table 2). This served as a simulation for the additional travel burden that would be imposed on SA residents should the closest clinic be closed.
The analysis was iterated over each SA, allowing us to evaluate not only individual SA but also regional impacts across the study area.
Statistical analysis
Data analysis and statistics were carried out using R software25. Linear regression was used to assess the predictive power of rurality on additional travel.
Results
Geographic and GP clinic data
A total of 1287 SAs exist in the study area: 511 in County Clare, 517 SAs in Limerick and 259 in Limerick City (Table 1, Fig1).
A total of 122 GP practice clinics were identified within the study area: 40 in County Clare, 48 in County Limerick and 34 in Limerick City (Table 1, Fig2). Additionally, 26 GP clinics outside but close to the border of the study area were identified.
Table 1: Mean area, mean population per Small Area, and Small Area count for County Clare, County Limerick and Limerick City classified by rurality index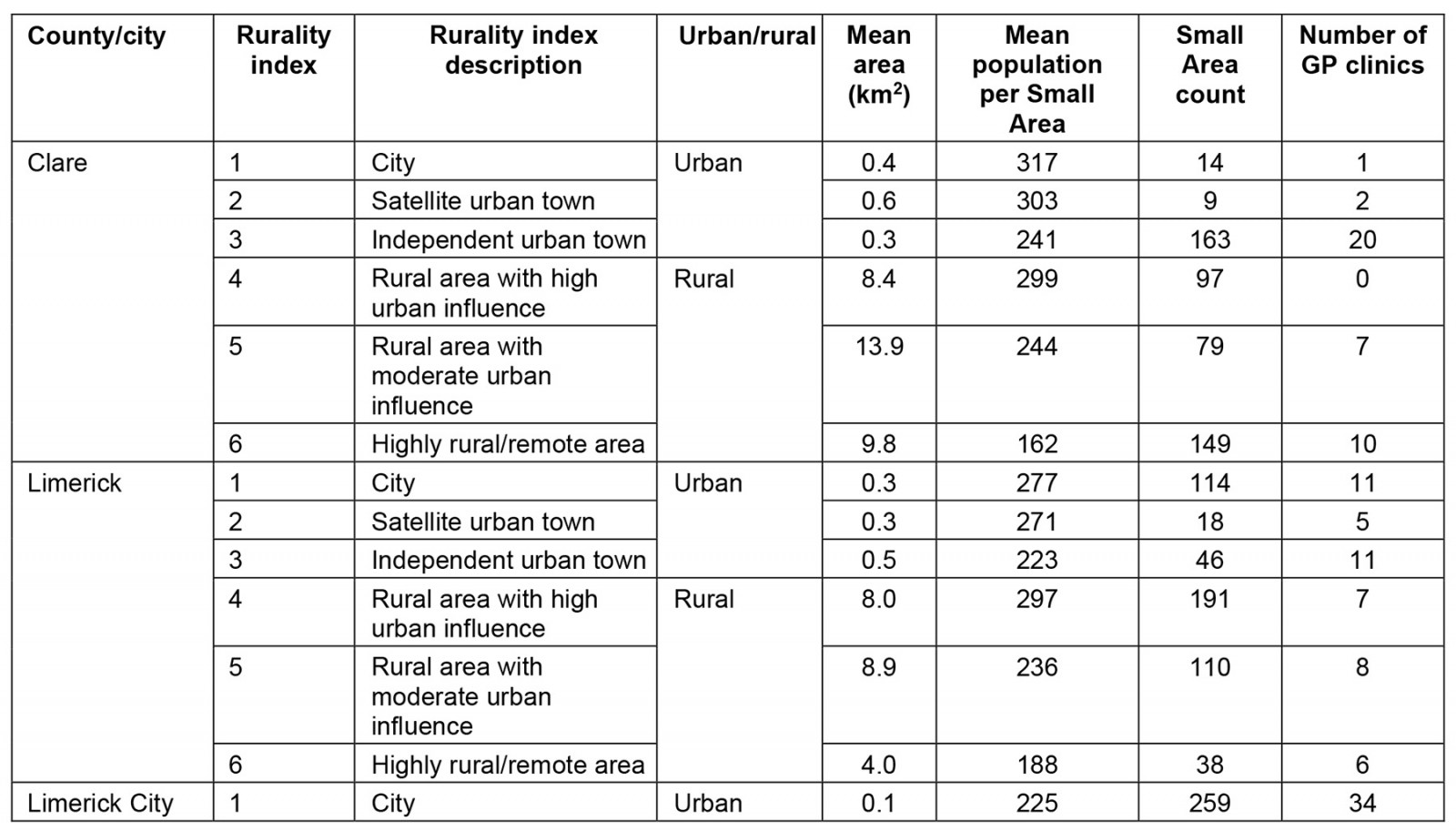
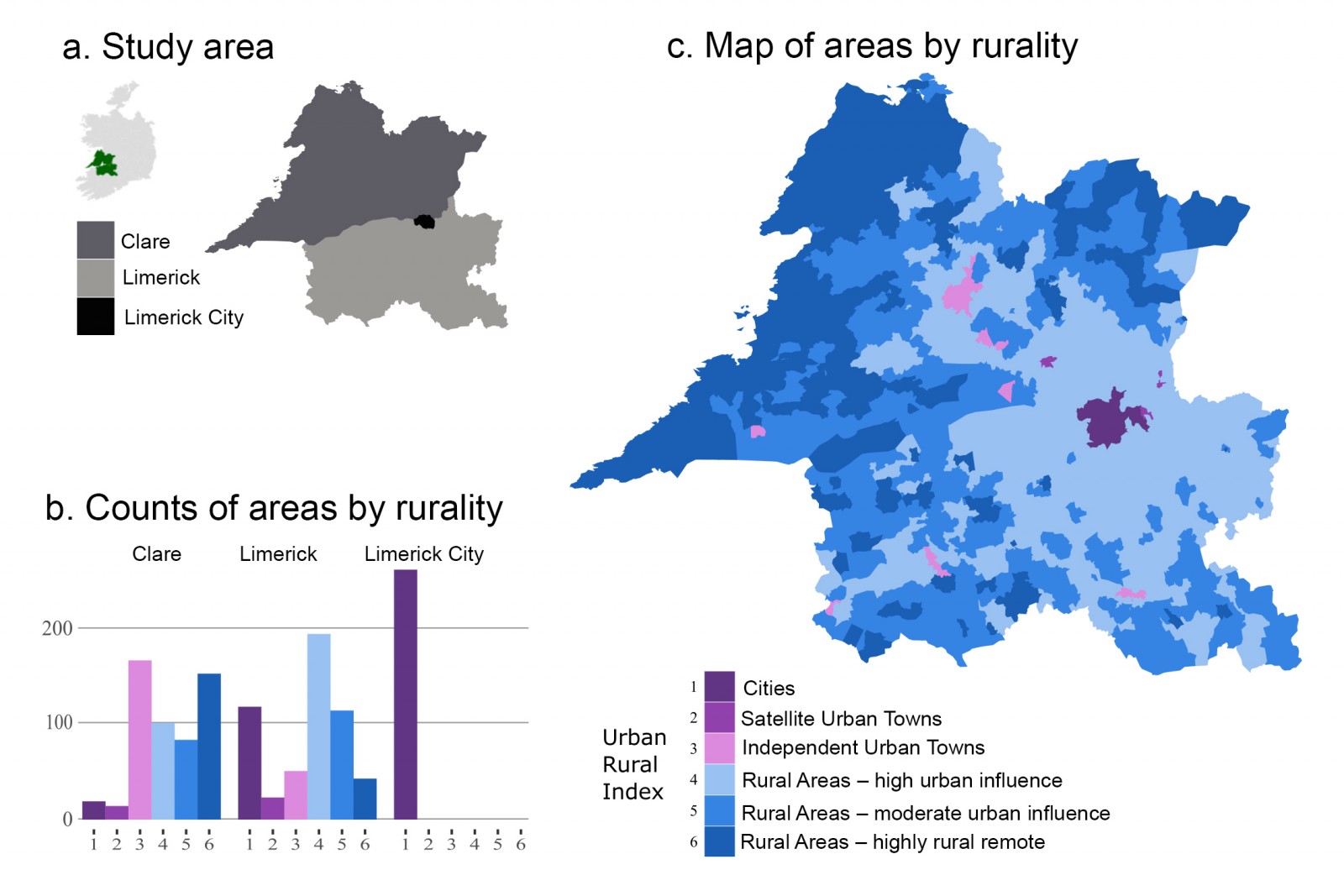 Figure 1: (a) Map showing location of study area within Republic of Ireland (green) and divisions of County Clare, County Limerick and Limerick City. (b) Bar chart showing number of Small Areas per study area. (c) Heat map of Small Areas classified on level of rurality.
Figure 1: (a) Map showing location of study area within Republic of Ireland (green) and divisions of County Clare, County Limerick and Limerick City. (b) Bar chart showing number of Small Areas per study area. (c) Heat map of Small Areas classified on level of rurality.
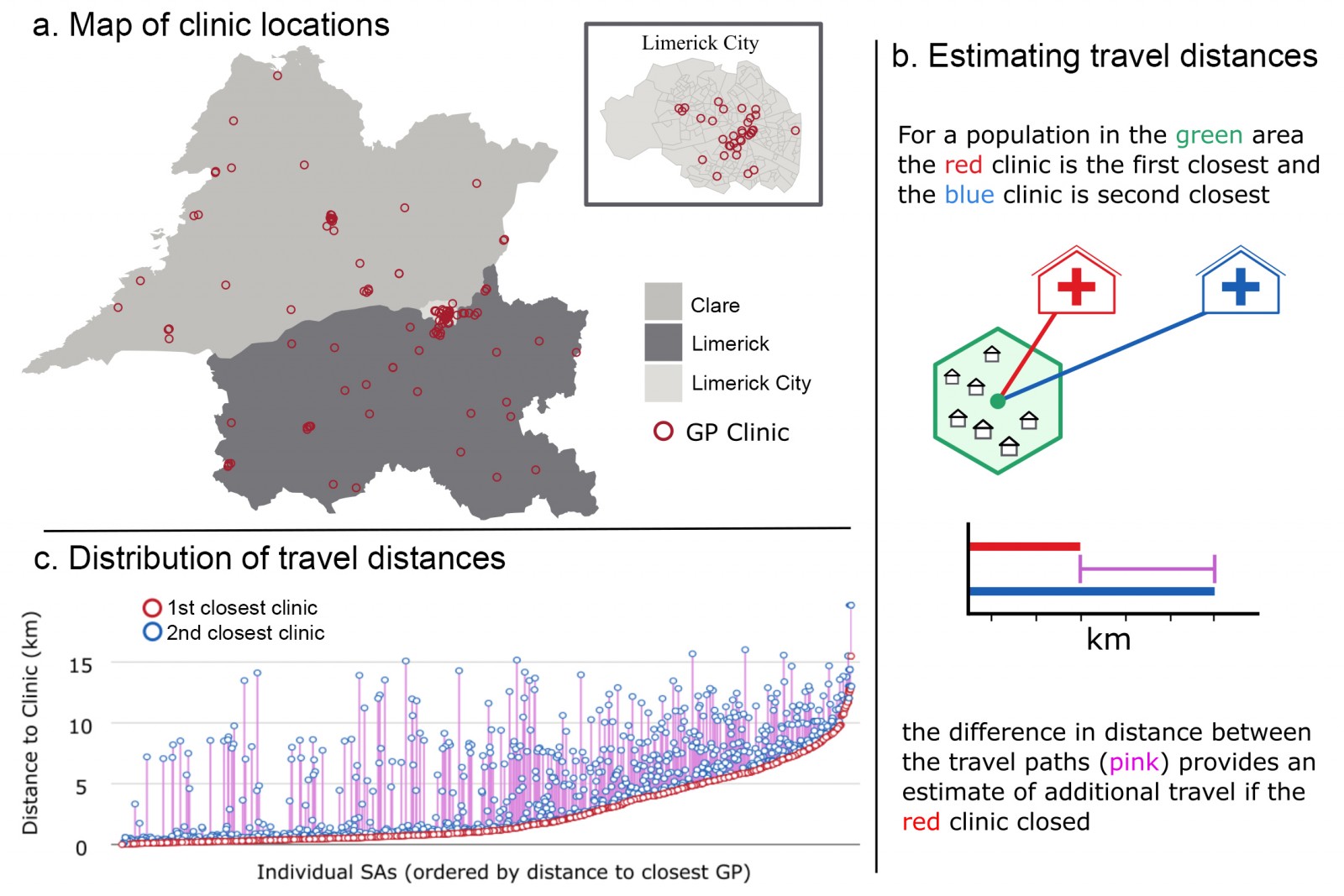 Figure 2: (a) Map showing location of GP clinics across County Clare, County Limerick and Limerick City. (b) Schematic representation of calculations for nearest clinic travel distance and new additional travel distances after clinic closure. (c) Overview of all estimated additional distances for Small Areas in the study.
Figure 2: (a) Map showing location of GP clinics across County Clare, County Limerick and Limerick City. (b) Schematic representation of calculations for nearest clinic travel distance and new additional travel distances after clinic closure. (c) Overview of all estimated additional distances for Small Areas in the study.
Rurality indexing
SAs in County Clare and Limerick were indexed into six levels of rurality. Of the SAs in County Clare, 325/511 (63%) SAs were classified as rural (rurality index 4–6) and, in Limerick, 339/517 (66%) were indexed as rural. Within Limerick City, 259/259 (100%) of the SAs were defined as being urban cities, with a rurality index of 1 (Table 2). Highly rural/remote SAs represented 187/1287 (15%) of all SAs across the study area, with 149/511 (29%) and 38/517 (7%) in County Clare and Limerick respectively.
Table 2: Travel distances to the nearest GP clinic and new additional distances after nearest clinic closure for SAs in County Clare, Limerick and Limerick City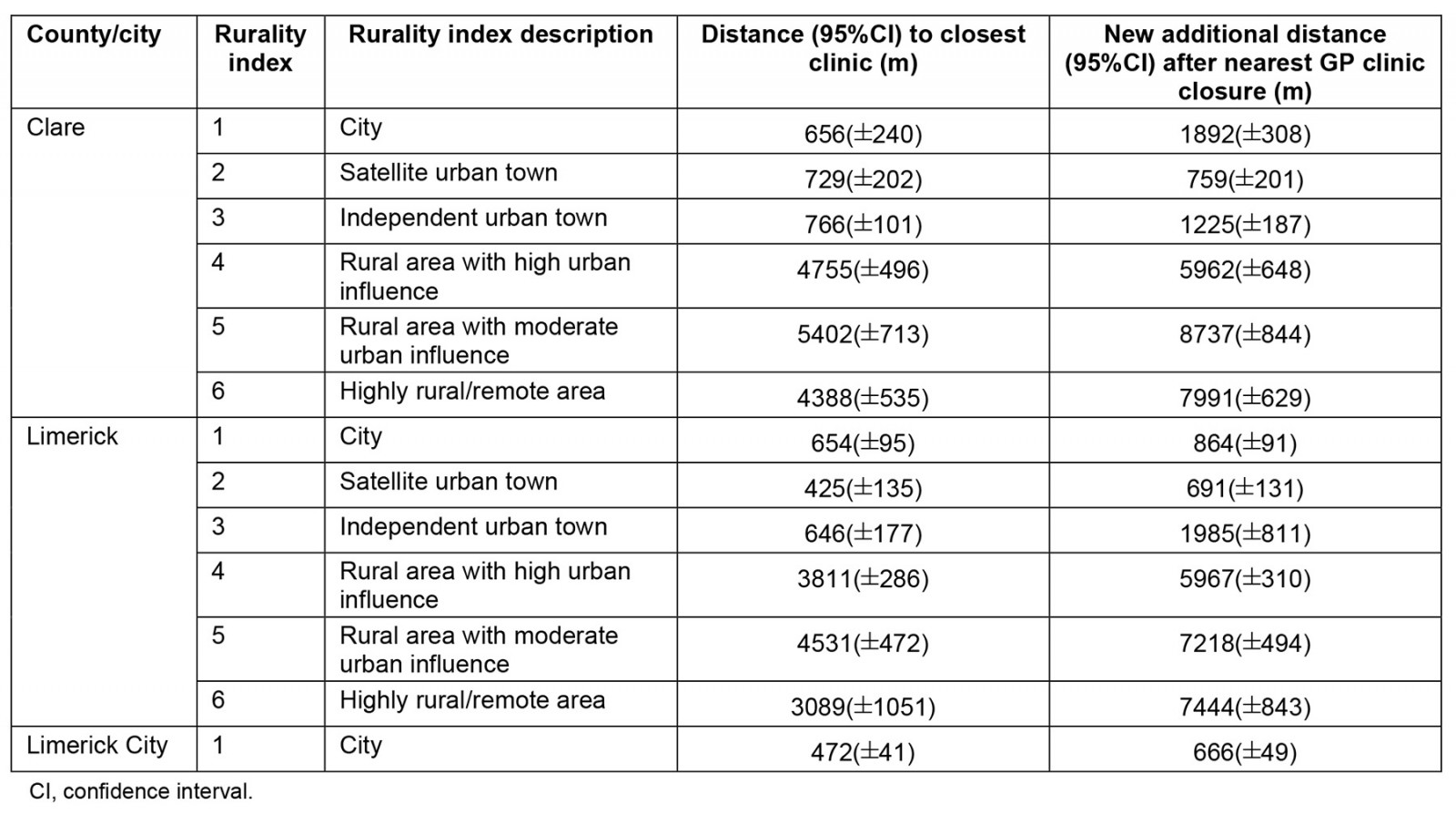
Travel distances to GP clinics
The average distance for all SAs to their closest GP clinic was 2530 m (95%CI ±150 m). In County Clare, the average travel distance for all SAs to their closest clinic was 3290±270 m; 2820±220 m in Limerick and 470±40 m for SAs in Limerick City. Rurally defined areas (rurality index 4–6) had higher travel distances than areas classified as being urban (rurality index 1–3). For all rurally defined SAs in the analysis, the average distance to the closest GP clinic was 4350±210 m, and for urban-defined SAs the average travel distance was 600±40 m (Table 2).
Travel distances to GP clinics after simulated closure: To model closure of each GP clinic closest to an SA (Table 2, Fig3), the difference between the original travel distance and the new distance to the second closest clinic was measured for all SAs. The average new additional travel distance across all SAs in the analysis was 1570±140 m (Table 2). The average new additional travel distances across County Clare were 1980±270 m, 1803±200 m in County Limerick and 200±30 m in Limerick City (Table 2).
For rurally defined SAs the average distances to the second closest clinic were 7040±250 m, whereas urban areas had new average distances of 980±90 m. As such, after simulated GP clinic closure additional distance also showed an urban rural split: average added distance for rural SAs was 2700±230 m compared to 370±70 m for urban SAs. The added distance was most prominent for highly rural and remote areas (rurality index 6), where average new estimated distance across both counties for these areas was 3760±500 m.
We carried out regression analysis using rurality to predict additional distance to a GP should the closest clinic close. The model also controlled for the current distance to the nearest GP. The model predicted that, for each additional step up in rurality, one additional kilometre of travel could be expected (982 m (95%CI 902–1063 m), p<0.0001). Overall, the model predicted about 30% of the variability in additional travel time (adjusted r2=0.31).
Figure 3c represents level of rurality and new travel length. Stepwise increase in travel distance is observed for increasing urban-rural index scores. Visual analysis shows the highest amount of variance in added travel time for increasing level of rurality (Fig3).
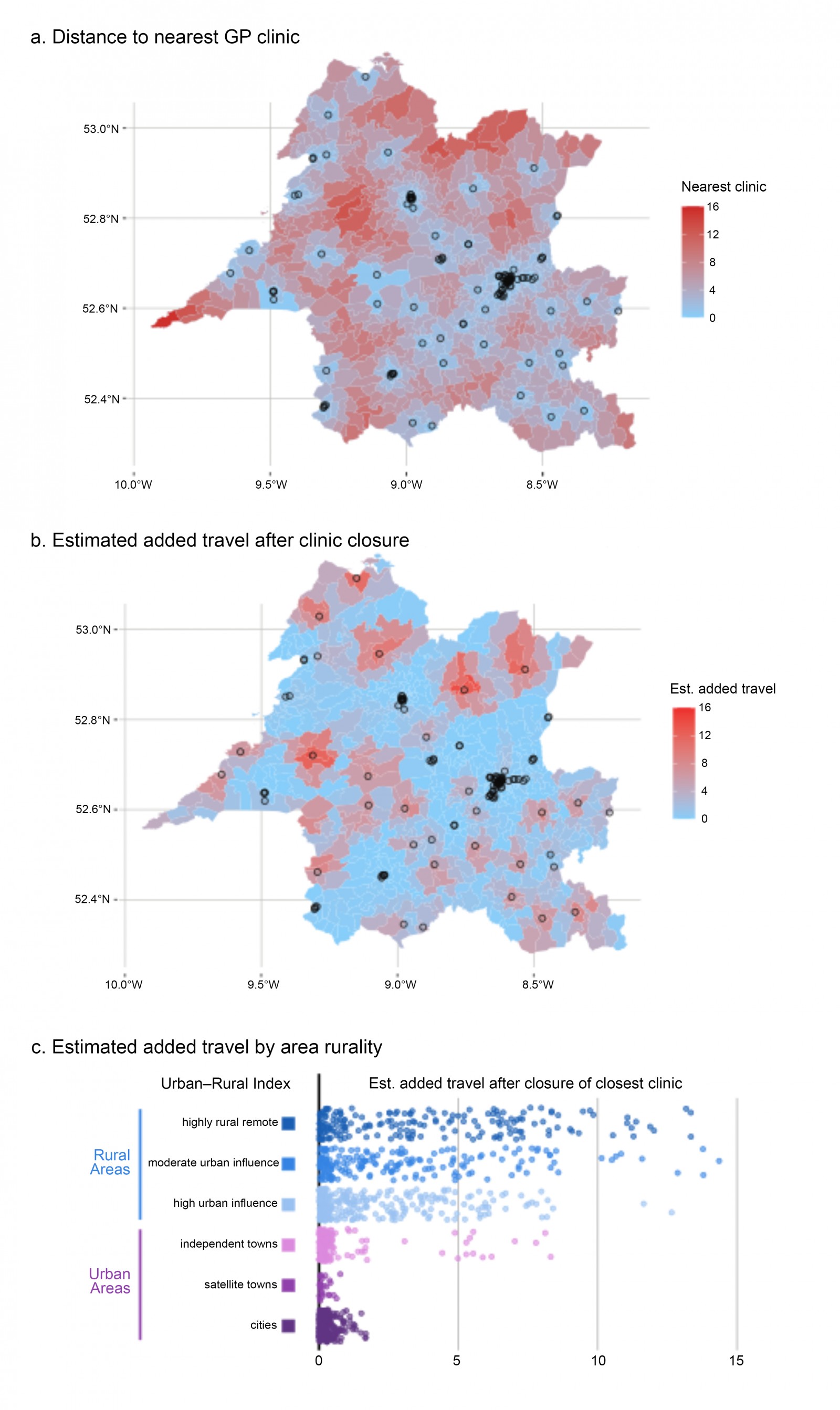 Figure 3: (a) Map showing location of GP clinics, with Small Areas coloured for distance (km) to nearest clinic. (b) Map showing location of GP clinics, with Small Areas added for estimated added distance (km) after nearest clinic closure. (c) Overview of the estimated new additional travel distances (km) for all Small Areas in the study population, indexed by level of rurality.
Figure 3: (a) Map showing location of GP clinics, with Small Areas coloured for distance (km) to nearest clinic. (b) Map showing location of GP clinics, with Small Areas added for estimated added distance (km) after nearest clinic closure. (c) Overview of the estimated new additional travel distances (km) for all Small Areas in the study population, indexed by level of rurality.
Discussion
Main findings
This study demonstrates and quantifies the increased distance that rural and remote populations have to travel to access GP clinics compared to those living in more urban areas. Travel distances increase in a stepwise fashion with the rurality of a community.
In addition, our study demonstrates that, the more remote a community, the greater the distance people will have to travel to the next closest GP clinic should their current closest clinic close. This may be expected given the lack of GP clinics seen in rural areas (Table 1).
Limerick City has a relatively small footprint and far more GP clinics compared to more rural areas in the county, and thus travel distances in the city are much shorter. The GP clinic distribution in County Clare was not as expected for level of rurality, as the most rural areas in County Clare had more GP clinics than their urban County Clare counterparts (Table 1). However, in highly rural and remote communities in both counties, the increase after the nearest clinic closure was more than double the overall average and more then 10 times the average increase seen in urban areas. These distances also tend to increase in a stepwise fashion with increasing rurality.
Our findings highlight the current geographical barriers that rural communities in Ireland face in terms of having to travel further to access GP clinics and services, and in relation to increased vulnerability to clinic closures. These findings confirm that rural community geographical isolation and limited GP clinic options make these areas particularly prone to GP clinic closure.
Comparison to existing literature
Ireland has one of the highest rates of rural-dwelling communities in Europe4. Previous research in the US has shown rural communities have to travel two to three times further to seek primary and secondary health care compared to their urban counterparts. Worryingly, patients with cancer, heart disease, depression or those who required complex surgical treatment needed to travel the furthest26. The same findings highlighted that rural communities often do not have any access to urban healthcare facilities26.
Similarly, data in Peru suggest rural communities compared to urban cities had a 1.9-fold increase in travel times to primary healthcare facilities and a 2.3-fold increase for secondary healthcare facilities27.
Our study focused solely on access and travel distances to primary care services rather than secondary health care. However, our data parallel previous research as the distance to GP clinics for rural-dwelling populations is seven times higher than for those who live in urban areas.
Our data indicate that Limerick City SAs are far more likely to contain a GP clinic than other SAs in this project. For rural and remote areas in our analysis, clinics are scarcer, and thus patient autonomy to choose a specific clinic is limited.
In the UK, data showed the highest travel distances and travel times to hospital and primary care clinics were in rural areas28. Our findings on clinic closure are congruent with previous research exploring the effects of healthcare clinic closure in rural areas.
For example, rural hospital closures in the US have result in increased mean transport and total emergency medical services activation times29. Single rural hospital closures in rural counties in the US have been shown to reduce community per-capita income and increase the unemployment rate30. There are several factors that may lead to the closure of a GP clinic. These include doctors retiring, practices with two or more doctors compared to a single doctor, high medical costs among patients and practices low in women and younger populations31.
GP clinic closures may also impact house-call visits. Data show house calls are more common in elderly patient populations and also more common in rural areas32. Recent research shows that house call rates are more common among older GPs compared to recent graduates, and house-call rates are more common among rural GPs compared to their urban counterparts33. House-call rates are declining in the Republic of Ireland, and visits may be essential for patient wellbeing and health outcomes34.
The closure of GP clinics has a considerable impact on the practice population, particularly on older patients. When a practice shuts, older patients may be content to move to a new clinic that is relatively close by, but dislike changing GPs. On the other hand, if they move clinic in order to retain the services of the same doctor, they value retaining the doctor–patient relationship but are unhappy with the increased travel35. In summary, clinic closure discommodes served populations. Nearby alternatives might not be suitable due to existing workload and workforce issues in general practice, distance and transportation issues. Hence, maintaining access to existing rural GP clinics is vital to meet health needs and provide accessible GP care locally.
Policy considerations
More must be done to address the gap in health equity for rural communities in the Republic of Ireland. Over the past 20 years in Ireland, the total number of GPs is increasing; however, the number of rural GPs is decreasing36. This is not a local phenomenon, and it is well documented that primary care providers tend to gravitate towards working in urban areas. Indeed, rural Irish GPs tend to be older than the GP national average: recent census data shows that 24% are over the age of 60 years and 14% are older than 65 years37. Difficulties in GP recruitment, short- and long-term cover and replacements, and poorer rural infrastructure contribute to a complex and worsening situation for rural GPs38.
There exist several opportunities in government policy and healthcare management plans to enhance equity for healthcare access for rural and remote communities across Ireland.
Financial incentives are one of the few health policy interventions intended to improve the distribution of GPs in rural areas39. Extensive postgraduate healthcare training in rural and remote areas as well as loan repayment options have been shown to retain rural healthcare workers40. Loan repayment options have been shown to be superior for retaining rural physicians compared to visa waivers; however, the issue appears to be complex, and should involve measures integrating health workers’ families into rural communities to enhance retention41.While there is a rural practice allowance scheme in Ireland, its strict criteria, modest budget and limited application have done little to stem the flow of younger GPs to urban centres.
Travel in Ireland is predominantly by car, averaging at 69% nationally42. In rural Ireland, 80% of trips are taken by car compared to 58% of those living in cities42. Approximately 32% of city dwellers walk for transportation compared to 8% of those in rural areas42. Public transport, including bus and train, accounts for approximately 4% and 1% respectively for a travel purposes42. A total of 68% of rural citizens report having no public transport tickets, 13% lower than the national average42. For comparison, 14% of a rural dwellers report they are within a 15-minute walk to their nearest doctor’s surgery, whereas 78% of those living in Dublin and the surrounding suburbs report living within walking distance42. The recent census data highlight that those living in rural areas are much more heavily dependent on cars for transport than any other region in the Republic of Ireland, rely less on public transport and walking, and are more likely to travel longer distances to all destinations including shops, restaurants, healthcare services and bus stops compared to the national average. The Republic of Ireland has implemented the Rural Transport Programme to combat the issue surrounding rural access and exclusion. The program includes door-to-door bus services and subsidised group travel to transport rural dwellers to cities and access other essential services. Expanding this program to include community car schemes is planned.
Mobility rates of GPs are generally low in urban areas but tend to increase with rurality43. Data from the US suggest that the majority of GP mobility begins early in GP careers, becoming more stable during the mid–late career years44. Thus, financial incentives should be directed at medical students and early-career GPs to incentivise rural practice. Data in Australia suggest higher financial pay increases incentives for newly trained GPs to work in rural areas; however, the effects on waiting times for patients are mixed, and financial incentives alone are not sufficient to increase access to rural primary care45. Currently, there are no additional government incentives in Ireland to increase the prevalence of rural GP practitioners. Specific rural medical curriculums and pathways should exist to enhance exposure of medical students and newly trained physicians to rural areas. Therefore, GP training schemes should include rural exposure to give new doctors experience of the complexities that rural patients present with. These training practices should expand to nursing students, pharmacists and all other medical care workers in primary care to close the gap on health access inequities38.
Study limitations
Importantly, there was an assumption that individuals used the clinic closest to them. There are limited data on this subject in the Irish context; however, recent data out of New Zealand shows that bypass rates may be as high as 60%46. There appeared to be a sigmoidal curve in the bypass rates: they were lowest when an individual lived closest to a clinic and highest when their clinic was further away. However, as Irish GP care provision is traditionally provided via the General Medical Services contract, which limits patient choice by their geography, bypass rates in the Irish context are not expected to be this high. Nonetheless, this requires further investigation to achieve a more accurate analysis of who uses certain GP facilities in the Republic of Ireland.
Another limitation to the study is that we are assuming that, should a GP clinic close, the next practice is able to recruit new patients. At present, approximately 79% of practices in the Republic of Ireland have their patient list closed37. We feel that highlighting areas where pressure to take on new patients will be felt most keenly is still possible and worthwhile using our methodology. We also understand that bypass rates can be significant in other jurisdictions, and a better understanding of these rates in the Irish context would add further richness to our analyses46. However, this requires further study as no central accessible list of patient addresses/locations (and indeed their chosen GP) is currently available to researchers in Ireland. However, we think that bypass rates are unlikely to be extremely high because the Irish system traditionally followed geographic lines: until 2011 GP lists included distance codes, which gave healthcare planners an incentive to place patients with GPs that worked relatively close by. The Health Service Executive can assign patients to new practices without the expressed agreement of the treating GP; however, these tend to be few in number (<10 000)47.
Another important limitation is that we did not account for single-handed or multi-GP clinics in our analyses. Thus the assumption that patients could just receive care in the next-nearest GP clinic is a gross over-simplification. Nevertheless, despite these limitations related to bypass rates and capacity issues in GP clinics in the Republic of Ireland, it is fair to say that if a clinic closes no patients will be able to receive care there, and thus the methodology here is a valid means to assess regional vulnerability to practice closure.
All travel distances from SA centroids to GP clinics were calculated as a minimum direct linear distance. We did not have access to a spatial interaction model to determine average travel distances and times within an SA to the nearest GP clinic using road networks or public transport. Thus we were unable to include travel time in our analyses. Further research should include data on travel time and not just linear distance to healthcare facilities, which is likely to be relevant to our rural areas with poorer road infrastructure and limited public transport links.
Conclusion
People in rural and remote communities in Ireland may have to travel more than 10 times further than their urban counterparts to access their GPs. GP clinics are most densely located in urban cities and towns, and travel distance to GP clinics increases with increasing level of rurality in a stepwise fashion. Moreover, rural populations will be most adversely affected by GP clinic closure in terms of increasing new additional travel distance, with the most remote populations being affected to the greatest degree. Rural communities, GPs, academia and policymakers will need to actively collaborate to ensure high-quality accessible and equitable health care remains possible in rural and remote areas.
Funding
No funding was received for this research.
Conflicts of interest
The authors declare no conflicts of interest.



