Introduction
Dental caries is one of the most prevalent and preventable diseases among Australian children1,2. Untreated dental caries causes pain, distress, illness and is a leading cause of preventable hospitalisation2. Children in the Northern Territory (NT) experience a higher prevalence of dental caries than children who live in other parts of Australia2,3. Aboriginal children residing in remote and very remote areas are disproportionately impacted by dental caries compared with their non-Aboriginal counterparts4. Of the NT Aboriginal children who received public dental services in 2022, 87% of children aged 11 years had experienced dental caries, and children aged 7 years experienced dental caries in 5.3 teeth on average4.
Community water fluoridation (CWF) is a widely recommended public health intervention to reduce dental caries5. CWF provides protective benefits through systemic administration of fluoride during amelogenesis in utero and during childhood, and through topical effects by increasing concentrations of fluoride in saliva to inhibit enamel demineralisation, promote remineralisation and inhibit bacterial action6-8. CWF is the addition of fluoride to drinking water supplies at levels known to benefit dental health5. Duration of CWF exposure is inversely associated with caries experience6,7. In Australia, CWF began in the 1950s and has made a significant contribution to improve oral health5. Rates of population access to fluoridated drinking water vary across Australia, with the NT having a higher proportion of the population without access to fluoridated drinking water (22%) than the national average (11%)3,5. While many communities in the southern region of NT access groundwater with naturally occurring fluoride at therapeutically beneficial levels, seven locations in the NT have implemented CWF: Darwin, the remote township of Katherine and five very remote communities (Angurugu, Maningrida, Umbakumba, Wadeye and Wurrumiyanga) among 205 remote communities9,10. For the five very remote communities to have implemented water fluoridation in 2013–14, all projects were community-initiated, facilitated by government community development grants.
Unlike other Australian states and territories, water fluoridation in the NT is not underpinned by legislation. The National Health and Medical Research Council (NHMRC) identified optimal levels of fluoride in drinking water for protective oral health benefits of 0.6–1.1 mg/L5. A longstanding NT policy on water fluoridation, introduced by the NT Department of Health in 201011, used population cost–benefit analysis to recommend that communities should be considered for prioritisation of CWF where the local population is greater than 600 people and natural levels of fluoride in drinking water supplies are less than 0.5 mg/L12. An updated cost–benefit study of CWF in remote NT communities, carried out in 2023, indicates that the population threshold in favour of cost-effective implementation of CWF is communities of 300 people or more13. While the cost–benefit study demonstrated clear economic benefits in broadening CWF in NT, it did not seek to examine causal inferences between CWF implementation and child dental caries, nor to understand how CWF may impact the trajectory of dental caries experience with age for children in remote NT communities. A deeper understanding of how CWF may impact dental caries in remote NT children throughout the course of childhood is essential to underpin life-course approaches to future government policymaking, investment and program design.
The present study aimed to understand the long-term impacts of CWF on children living in remote and very remote communities of the NT. In doing so, this study sought to demonstrate the use of a difference-in-difference (DiD) analysis as a means of policy evaluation, to quantify the impacts of a longstanding NT Health CWF policy, by measuring dental caries experience in NT children aged 1–17 years living in remote and very remote locations between 2008 and 2020.
Methods
To inform the DiD analysis, a systematic approach was used for collection and sampling of secondary data. As the NT Government is the major longstanding provider of oral health services to most remote communities of NT, service data were the most comprehensive data source available. These data were collected at the point of service by dental practitioners, based on clinical examination. Each record also contained information about individuals’ demographic attributes, residential location, Indigenous status, age and dental caries experience.
The sampling strategy is outlined in Figure 1. For a total of 91 sites across the NT, consisting of 19 urban centres, and 72 remote and very remote Aboriginal communities, data for drinking water quality data collections for 2008–2020 were held by the Power and Water Corporation. Drinking water quality data from 75 localities were matched to the 50 remote community populations included in the study14. Data were cleansed of duplicate entries. Communities with fewer than 100 total observations were excluded to improve data quality and prevent inadvertent identification of individuals. To minimise confounding of results, individuals’ demographic information was screened for a change in location partway through the study period, and these records were removed from the dataset. The oral health data sample captured all children aged 1–17 years who had received dental care in remote and very remote locations of the NT from 2008 to 2020. For each unique patient record, dental caries severity was measured and reported using the decayed, missing and filled teeth index (dmft (primary teeth)/DMFT (permanent teeth)), which is a standard epidemiological measure of dental caries experience15. A dmft/DMFT score was collected per individual, per year (termed ‘person-year observation’) for all children in the sample.
Dental caries experience data were matched with water quality data. Tables 1 and 2 show the distribution of the study population in 50 remote and very remote communities. Of the total 64 399 person-year observations from 24 546 children, 73.6% (47 429) observations related to communities with fluoride levels at or above 0.5 mg/L, including 13 941 observations relating to the one remote community (Katherine) and five very remote communities with CWF (Angurugu, Maningrida, Umbakumba, Wadeye and Wurrumiyanga) and 33 488 observations relating to 12 communities with naturally occurring fluoride in drinking water supplies at therapeutically beneficial levels at or above 0.5 mg/L. The remaining 16 970 observations related to 32 communities with fluoride levels in drinking water less than 0.5 mg/L. Aboriginal children made up a higher proportion (63.2%) of the study population than non-Aboriginal children (36.8%).
The study used a quasi-experimental design. The DiD analysis is suited to evaluating population health impacts of historical interventions in non-randomised populations16,17. As CWF was implemented in remote communities throughout 2013–14, data were grouped into time periods prior to and including 2014 (pre-intervention) and after 2014 (post-intervention), factoring in a 12-month lag period for effects of ongoing fluoride exposure to be observed6,13. The treatment group comprised data from the remote communities that received the CWF intervention. To account for possible effects of naturally occurring fluoride in community water supplies, two control groups were used. Control group 1 included all data for communities that had naturally occurring fluoride in drinking water supplies at levels at or above the NT Department of Health policy threshold of 0.5 mg/L. The control 2 group comprised all data for communities that had naturally occurring fluoride in drinking water supplies below the level recommended by the Department of Health policy (<0.5 mg/L) (see Table 1).
Figure 2 presents the conceptual framework of the analysis, comparing the outcome (dmft/DMFT) for the pre–post time-point differences for the treatment and control groups, thus quantifying the differences between these groups that could be attributed to the effect of the CWF intervention. Analysis was conducted using statistical analysis software STATA v17 (StataCorp; https://www.stata.com)18.
Table 1: Number of communities, children, observations and fluoride levels for treatment and control groups, by pre- and post-intervention periods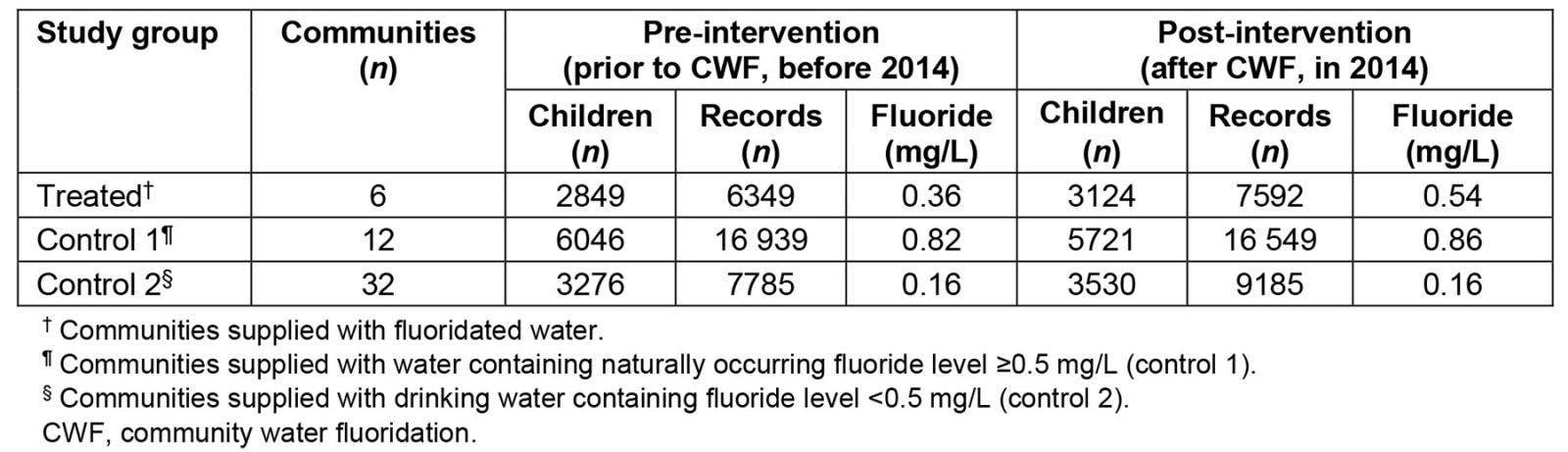
Table 2: Key demographic characteristics by treatment and control groups, Northern Territory 2008–2020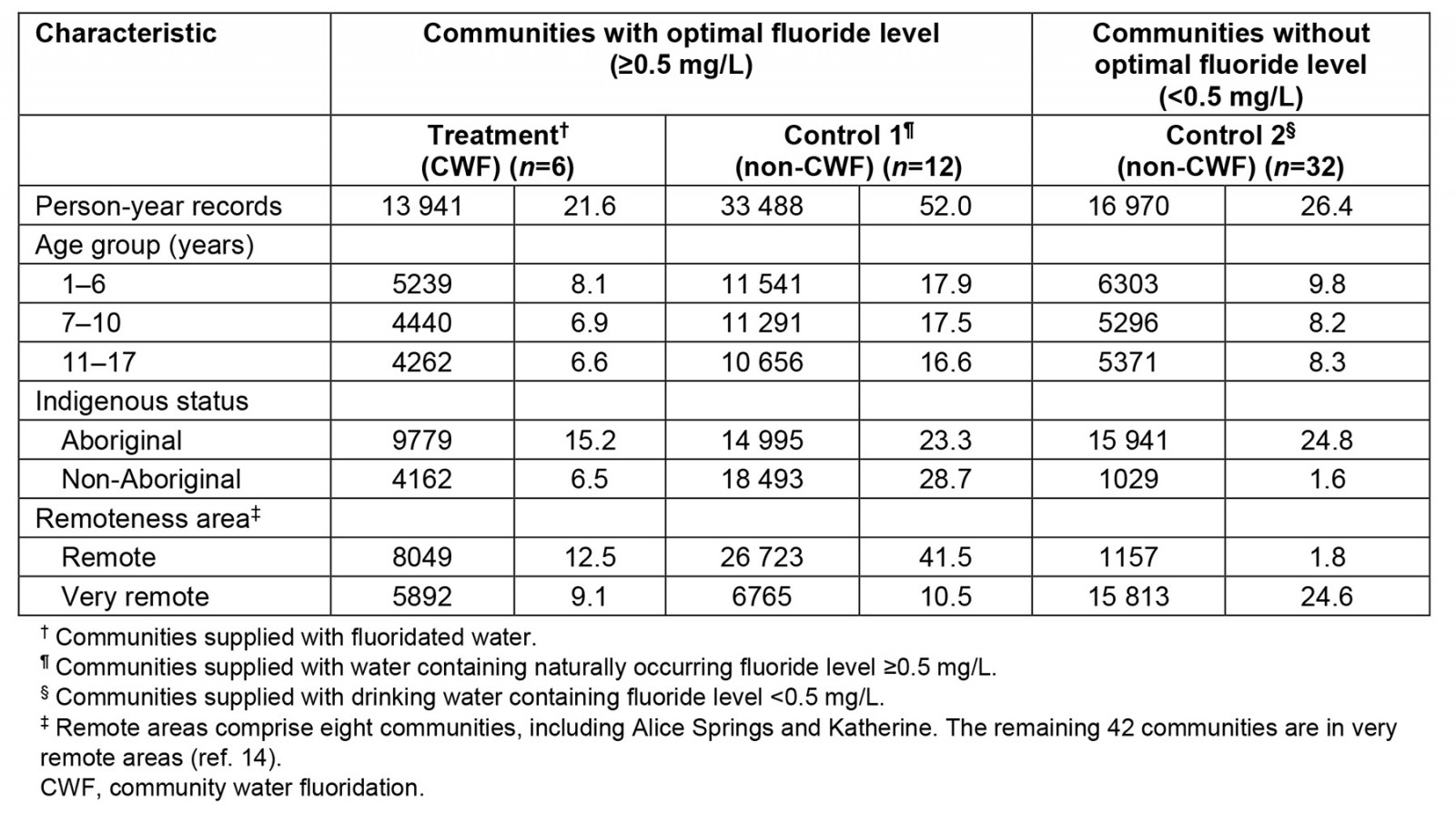
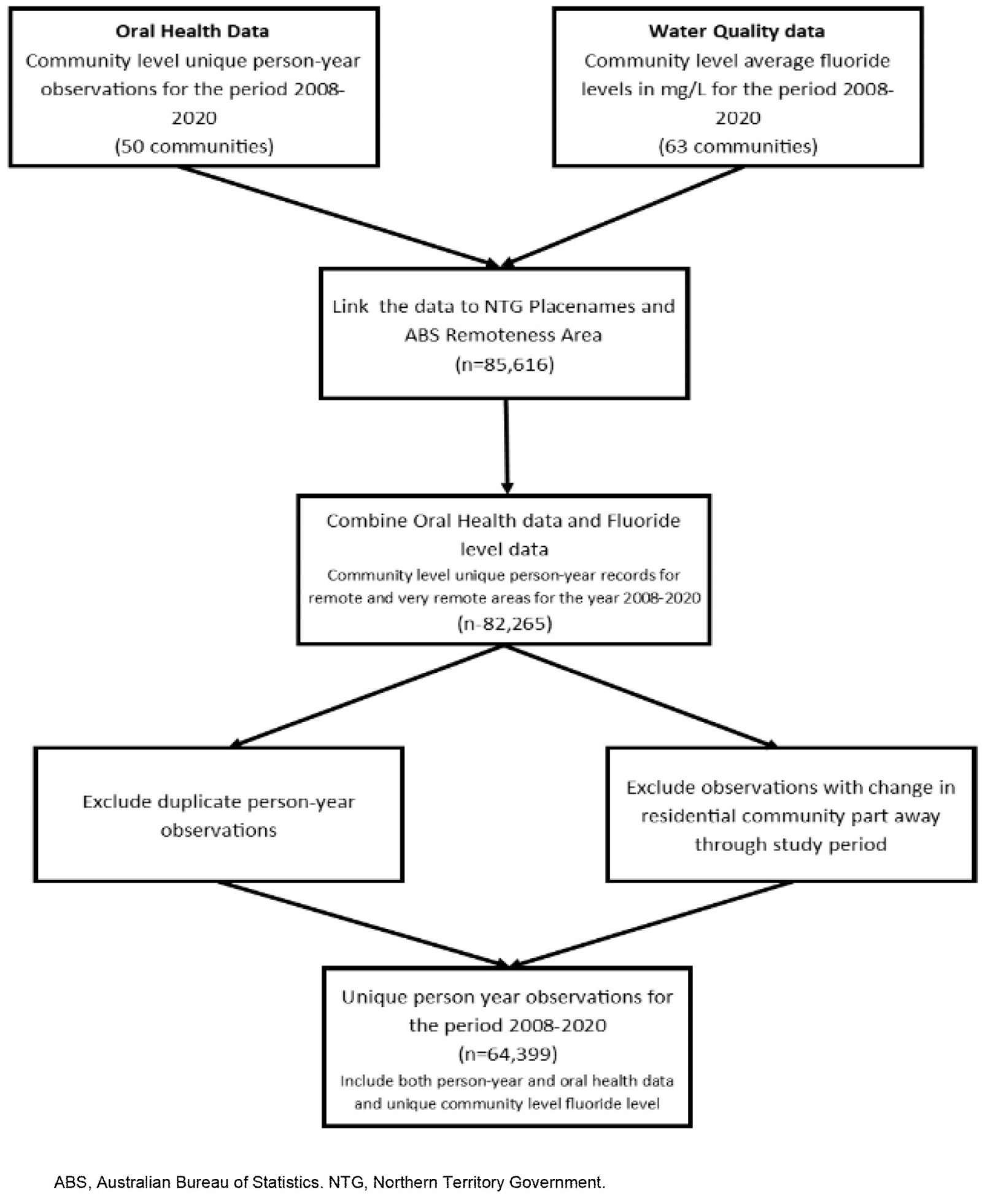 Figure 1: Data sampling strategy.
Figure 1: Data sampling strategy.
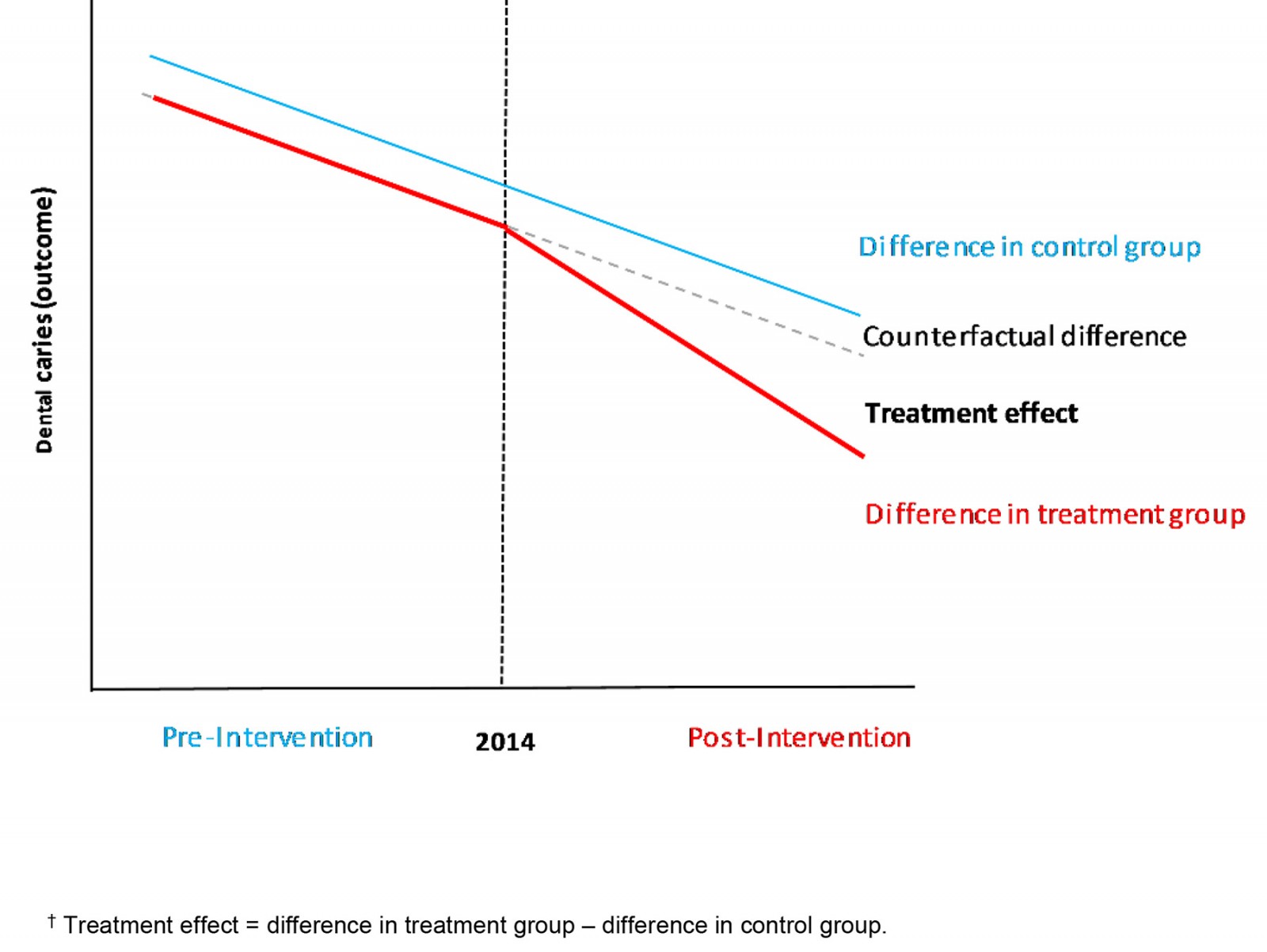 Figure 2: Difference-in-difference analysis conceptual framework for community water fluoridation.†
Figure 2: Difference-in-difference analysis conceptual framework for community water fluoridation.†
Ethics approval
Data were collected and utilised in accordance with the Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health Research ethics approval 2021-3988.
Results
For the total data collection period, from 1 January 2008 to 31 December 2020, the overall prevalence of dental caries in children aged 1–17 years was 62.1%. Aboriginal children experienced dental caries at a rate 1.7 times greater than non-Aboriginal children. The analysis found that 48.3% of children aged 1–6 years, 29.7% of children aged 7–10 years and 70.5% of children aged 11–17 years experienced dental caries in the primary, mixed and permanent dentitions respectively. Aboriginal children were also more likely than non-Aboriginal children to experience dental caries across all age groups, which was found to be statistically significant (p<0.01) for all age groups, except children aged 1 year. Figure 3 presents average dmft/DMFT for each of the treatment and control groups, before and after the CWF implementation period. While each of the treatment and control groups experienced general declines in dmft/DMFT over the entire study period, the magnitude of decrease was greatest for the treatment group.
Table 3 summarises results for each of the control and treatment groups and provides further demographic breakdown. Observed decreases in dmft/DMFT between the pre- and post-intervention periods were tested with a high level of statistical significance (p<0.01). The control 1 group had a generally lower average dmft/DMFT across all age groups in both the pre- and post-intervention periods, when compared to the treatment and control 2 groups. The average dmft/DMFT for the treatment group decreased to a greater extent than both control groups between the pre- and post-intervention periods. Children in the treatment group aged 7–10 years and 11–17 years experienced the greatest decreases in dmft/DMFT between the pre- and post-intervention periods. The control 2 group experienced the lowest magnitude of decrease in dmft/DMFT across all ages, except for children aged 1–6 years. Declines in dmft/DMFT were greater for non-Aboriginal children compared to Aboriginal children across all treatment and control groups.
Table 4 presents the results of the DiD analysis. Overall, the observed decline in the post-intervention period for the treatment group, compared with both control groups was 0.28 affected teeth (dmft/DMFT). In comparing the average dmft/DMFT for the treatment group and control 1 group, the post-intervention decline in the number of teeth affected by caries across all ages was on average 0.13 dmft/DMFT greater for the treatment group than the control 1 group. A greater post-intervention decline, of 0.30 dmft/DMFT, was observed for the treatment group when compared to the control 2 group. These results were tested with high statistical significance (p<0.01), summarised in Table 4. Notably, children of ages 7–10 years and 11–17 years in the treatment group experienced significantly greater post-intervention declines in average dmft/DMFT, by 0.32 and 0.40 fewer affected teeth respectively, when compared to the control 2 group (p<0.01). Children aged 1–6 years in the treatment group experienced statistically significant (p<0.01) post-intervention declines of 0.43 dmft/DMFT relative to the control 1 group, and 0.52 dmft/DMFT relative to the combined control groups.
Table 3: Dental caries (dmft/DMFT) for children aged 1–17 years, reported by age group, for treatment, control 1 and control 2 groups before and after community water fluoridation intervention, Northern Territory, 2008–2020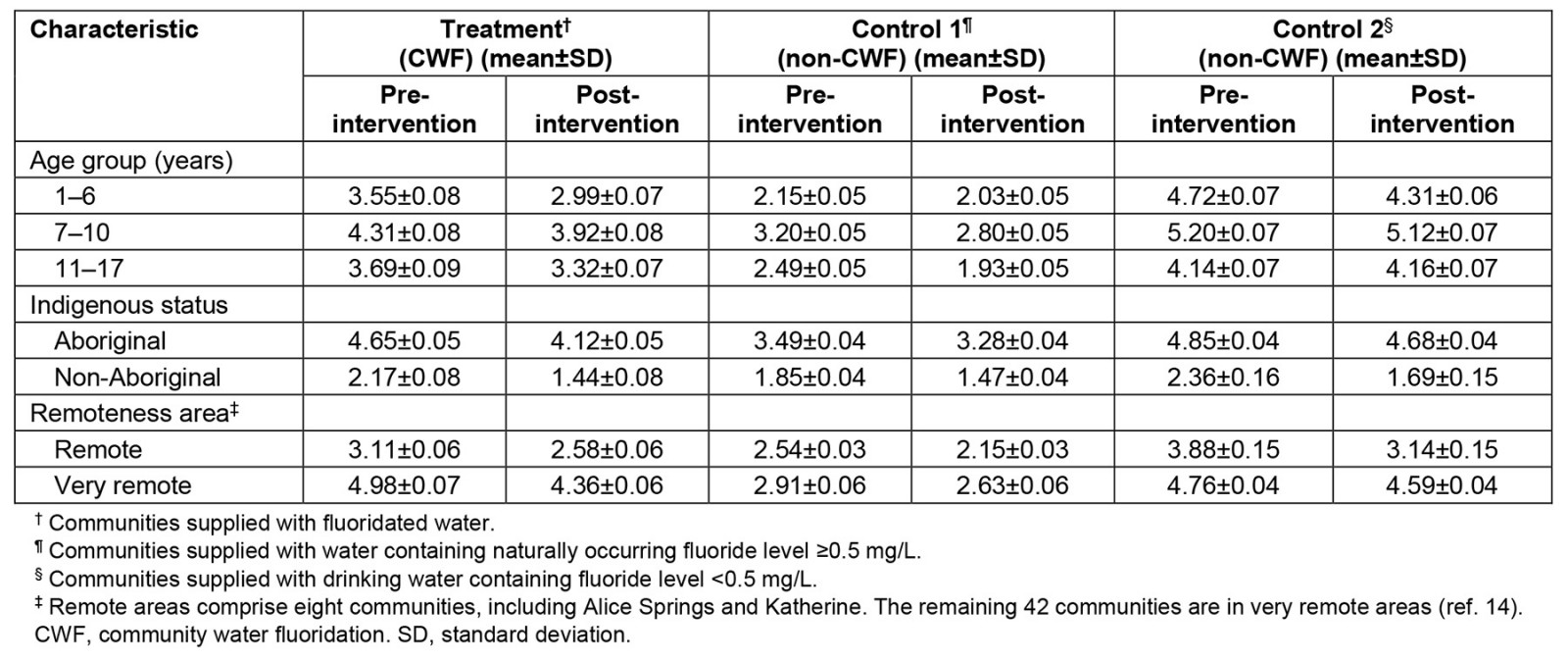
Table 4: Difference-in-difference analysis of dental caries (dmft/DMFT) for children aged 1–17 years, reported by age group, for treatment, control 1 and control 2 groups, Northern Territory, 2008–2020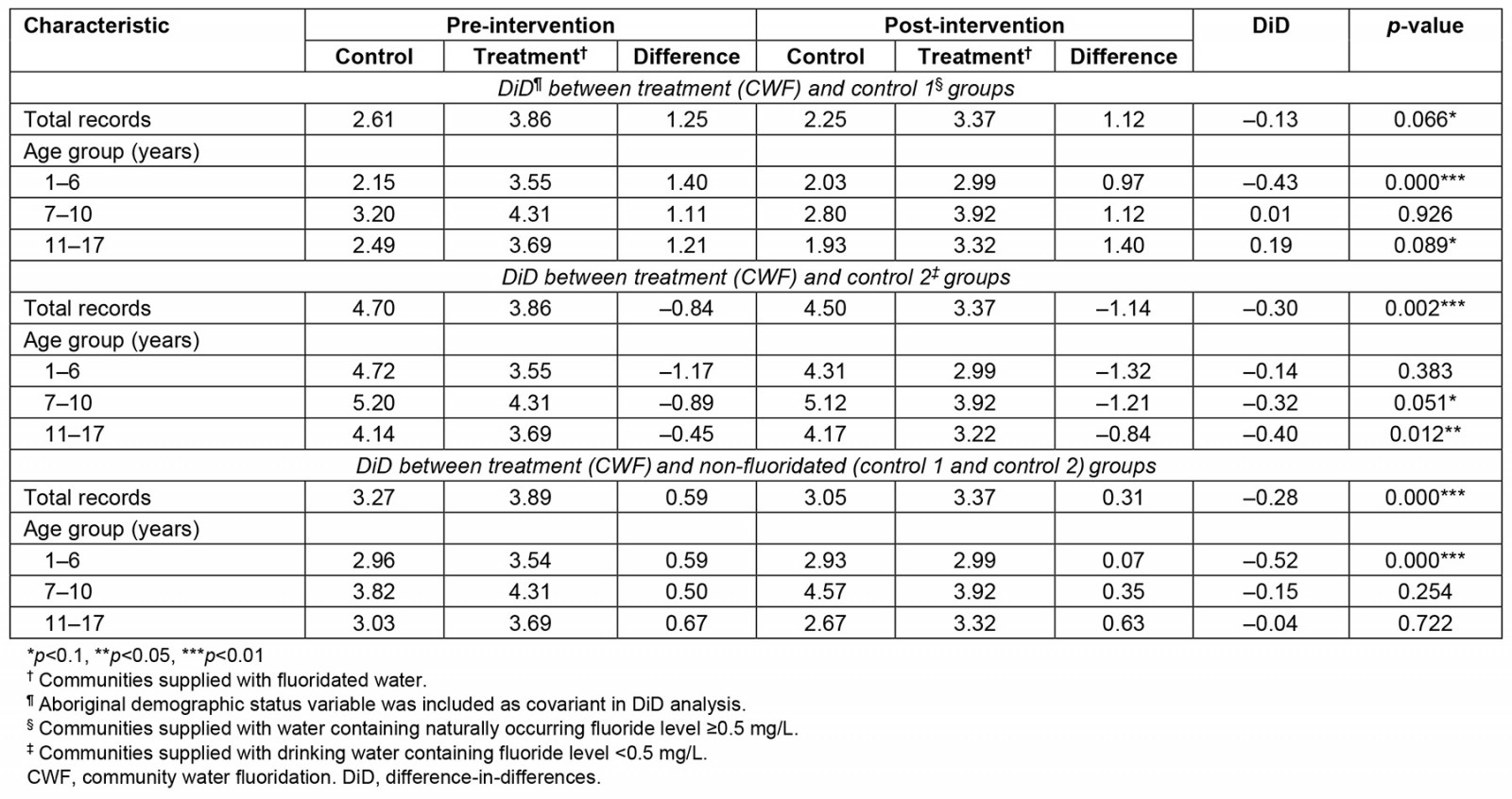
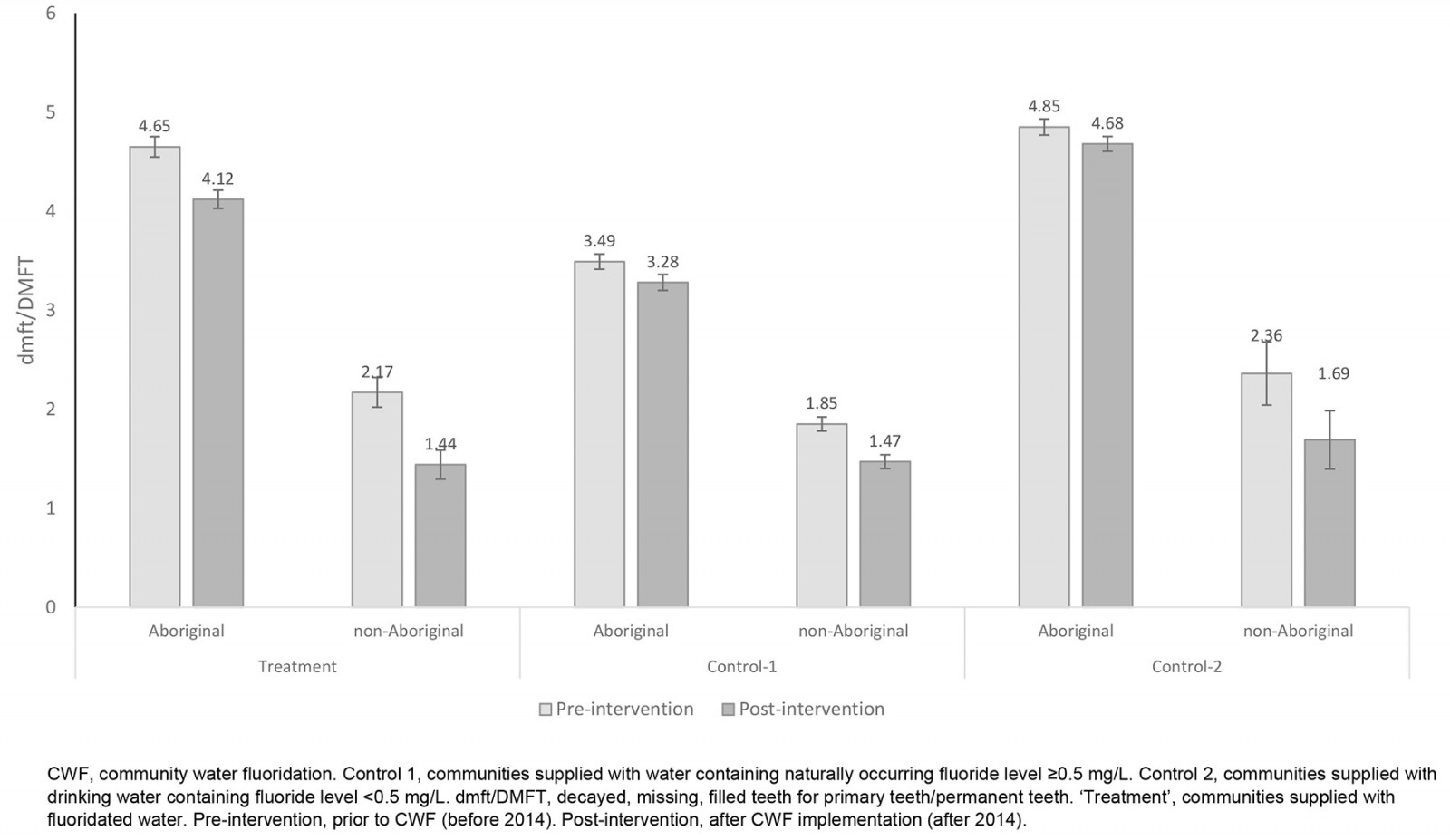 Figure 3: Dental caries experience (dmft/DMFT) at 95% confidence interval for treatment and control groups, for pre-intervention and post-intervention periods.
Figure 3: Dental caries experience (dmft/DMFT) at 95% confidence interval for treatment and control groups, for pre-intervention and post-intervention periods.
Discussion
Children of all ages in remote and very remote areas of NT are affected by dental caries at levels much higher than previously reported by national studies of child oral health1,4. It is clear that Aboriginal children residing in remote and very remote communities of the NT experience dental caries at levels well above their non-Aboriginal counterparts. Our study not only documented caries experience of remote NT child populations not previously included in sampling conducted by national studies1-3, but also demonstrates the effectiveness of CWF in reducing high levels of dental caries among child populations in remote and very remote NT, consistent with previous studies of water fluoridation in the remote NT19. Our study also identified overall decreases in rates of dental caries among the total NT child population over the study period, consistent with other analyses that have reported general improvements in child dental caries in NT and Australia over similar time periods20,21. Other factors, such as efforts to address social determinants of health, health promotion and better management of chronic conditions, may be having a degree of impact, as recent research on life expectancy of Aboriginal people in the NT has demonstrated general improvements over the past decade22. However, overall declines in the severity of child dental caries, measured by dmft/DMFT score, confirmed that populations that received CWF exhibit lower rates of dental caries.
Our study provides insight into the relationship between dental caries among the remote and very remote child populations of NT and levels of fluoride in drinking water. Regardless of CWF or naturally occurring fluoride sources, a clear inverse association exists between the number of teeth affected by dental caries in children and fluoride level in remote community drinking water supplies, consistent with data-linkage studies of other populations23. We did not seek to predictively model a dose–response relationship curve; however, our approach to hypothesis testing yielded an important finding. Children in NT communities with long-term naturally occurring fluoride in water supplies at levels at or above 0.5 mg/L experienced dental caries in fewer teeth on average, with a high degree of statistical significance. This finding supports evidence linking long-term duration of exposure to fluoride with better oral health outcomes6,7,23 and emphasises the importance of a life-course approach to preventive initiatives.
The DiD approach is emerging as a promising method in quasi-experimental analysis and public health policy evaluation24,25. Our study demonstrates the usefulness of the DiD method in policy evaluation by adopting a ‘natural experiment’ design, to assign individuals from similar communities to control and treatment groups depending on the CWF intervention received. The approach is useful in public health settings where stringent, randomised methods of testing population responses to a policy intervention may not be practicable. There are known limitations to the DiD method in health policy evaluation; the validity of results relies on equal background trends being established in control and treatment groups, so that all groups are subject to similar conditions and yield similar health outcomes over time, thus enabling observed changes in outcomes to be attributed to the policy intervention or treatment24. Based on our observations, parallel trends in caries experience (dmft/DMFT) were noted for the control 2 and treatment groups prior to CWF implementation. The control 1 group, exposed to naturally occurring fluoride in water supplies throughout the entire study period, had a lower baseline dmft/DMFT, but also experienced a gradual decrease in dmft/DMFT over time.
We accounted for confounders arising from variations in naturally occurring fluoride in water supplies by separating control groups into low levels of naturally occurring fluoride (<0.5 mg/L) and therapeutically beneficial levels of fluoride (≥0.5 mg/L). Our study utilised data collected over an extended period, thereby limiting the confounding potential of brief periods of changes in levels of services or situational community factors that may skew results over short periods of measurement. The extensive dataset related to children who accessed public oral health services within the study period. Of the current 27 000 Aboriginal children in the NT aged 0–18 years, 20 397 (75%) have accessed public dental services between 2012 and 20224. Thus, we believe our dataset to be reflective of the majority of Aboriginal children in the NT. The remaining proportion of Aboriginal children not captured by the dataset (25%) may be reflective of children not accessing any dental care, or accessing dental care through other programs, administered through the private sector or small number of non-government and community-controlled programs. As our study used oral health data pertaining to children who had contact with a single public oral health program, any changes associated with overall program service levels would also have affected each of the control and test groups similarly.
Our study did not examine exposure to preventive effects of fluoride from other sources. Two longstanding government programs underpin the use of concentrated fluoride varnish in NT children: the Healthy Under 5 Kids Partnering Families Program (HU5K-PF) for children aged 18 months to 5 years26 and the NT Remote Aboriginal Investment Oral Health Program (NTRAI-OHP) for remote Aboriginal children of all ages4. These programs are implemented at similar levels across remote and very remote NT communities, but have been limited in their overall continuity of fluoride varnishing at therapeutically indicated intervals27. Given the limited coverage of these oral health preventive programs over extended periods, it is unlikely that the use of fluoride varnish was a significant confounder in our analysis.
Our study did not account for dietary and behavioural confounders such as high consumption of sugar-sweetened beverages, which is known to be widespread in remote and very remote communities of the NT28,29. It is known that dietary and behavioural risk factors for oral disease, as well as access to culturally safe services, may disproportionately impact the oral health of Aboriginal people compared to non-Aboriginal people2. The treatment and control groups utilised by our study had different proportions of Aboriginal and non-Aboriginal people, which could have potentially confounded the analysis of the study data. Moreover, the treatment and control groups varied in overall population number and age structure. Due to the natural experiment approach to the study, it was not possible to control demographic composition between each of the control and treatment groups. However, the proportion of Aboriginal and non-Aboriginal people in each of the control and treatment groups remained relatively stable over the study period, as did population number and age structure, which is suited to the DiD focus on relative differences in population outcomes over time using a parallel trends assumption24,25.
Previous studies of CWF effectiveness have postulated that individuals in warmer climates are likely to consume larger amounts of water, and on this basis a suitable concentration of fluoride in drinking water may be at the lower end of the optimal range30. To be effective, CWF also requires drinking water to be safe and palatable for consumption. We did not account for differential rates of water consumption, which we assume to be generally similar across NT communities. Any inferences made from our analysis would be contingent upon drinking water consumption continuing at current rates. Our study also did not consider possible dose–response differences in dental caries within the optimally fluoridated range. Numerous NT remote communities have naturally occurring fluoride in water supplies at varying levels within the NHMRC-defined optimal range5,9,10. Further studies could assess the dose–response impact of higher levels of water fluoridation on dental caries severity over extended periods.
Our findings suggest that the longstanding policy position of the NT Department of Health, recommending CWF in remote and very remote communities with levels of naturally occurring fluoride in water at levels below 0.5 mg/L11, has supported improvements in oral health among child populations that experience high levels of dental caries. A case for extending CWF to other remote and very remote communities of NT, with lower levels of naturally occurring fluoride in drinking water (<0.5 mg/L), could be progressed on the basis of clear, predictable and cost-effective population health benefits. A recent cost–benefit analysis of CWF implementation in NT suggests that the economic return on investment can be as high as 16:1 for the NT’s largest remote communities, with a payback period as short as 2.2 years13. There are also clear synergies arising from co-investment by government in universal prevention offered by CWF in addition to targeted, settings-based preventive programs such as fluoride varnish programs, which have been tested in the NT child population. A previous study of dental caries in remote NT children31 estimated that the combined effects of a fluoride varnish program and CWF of 1 mg/L could produce an average reduction of 7.8 carious tooth surfaces per child. As critical health workforce shortages in remote and very remote Australia continue, cost-effective, universal health interventions that operate external to health service settings, such as CWF, will offer sustainable and predictable investment for governments to improve population health outcomes, reduce health inequity and reduce health system pressures.
Conclusion
Observed decreases in dental caries among children in remote and very remote NT communities demonstrate promising improvements in population oral health. However, rates of child dental caries, especially for Aboriginal children in remote and very remote NT, are still some of the highest in the country and affect these populations disproportionately compared to their counterparts in major cities. Children who receive adequate levels of fluoride in drinking water, irrespective of natural or CWF sources, experience dental caries in fewer teeth on average compared to children without access to fluoridated water. Overall rates of reduction in dental caries have been accelerated for NT remote child populations following the introduction of CWF.
This study adds to the sizeable body of evidence of clear benefits of extended CWF in areas where fluoride levels in drinking water are below optimal levels. CWF does not replace the need for complementary preventive programs and oral health promotion; rather, investment in CWF is likely to increase the impacts of other preventive efforts. Moreover, CWF is a cost-effective and sustainable health intervention that is not dependent upon a health workforce currently facing critical shortages, making it a sound investment in population health. Future CWF policy advancements in NT should focus on implementation, by working with communities to broaden the reach of CWF into remote and very remote areas where indicated. To assist prioritisation, future studies could consider regional trends in dental caries for NT children, relative to fluoridation levels.
References
You might also be interested in:
2018 - Lack of Medical Resources and Public Health Vulnerability in Mongoliafs Winter Disasters


