Introduction
Patients often prefer to see an experienced doctor because they worry that inexperienced doctors will not be able to provide them with suitable treatment1. It can therefore be a challenge for junior doctors, also known as interns, to establish good relationships with patients while acquiring the necessary clinical skills through practice2,3. Some studies have suggested that patients’ level of comfort with care provided by interns appears to differ with interns’ level of involvement and competencies, as well as other factors4-6. It has also been reported that community-based medical education could play an important role in not only nurturing clinical skills but also understanding community health care for interns and medical students7,8. Recently, both urban and rural or remote communities internationally have had reported benefits in terms of medical education from community-based clinical training9-11. Previous investigations have shown the importance of active participation of communities in understanding not only community medicine but also the whole community itself12. Some past studies have also suggested that these programs can benefit in primary care settings in particular8,13,14. However, few studies in medical education have investigated purely geographic or demographic elements, and especially those with a community resident perspective. It is not known whether there is an association between demography or geographic region and patients’ acceptance or attitudes toward care provided by interns15.
A new internship system started in 2004 in Japan, in which interns had to complete 6 months of training in internal medicine; 3 months in emergency medicine; and at least 1 month in each of surgery, pediatrics, obstetrics and gynecology, and community medicine, in 2 years training curricula. Before this, almost 90% of interns were trained in tertiary hospitals. Since 2004, approximately 60% of interns have chosen to start their internships in community hospitals, including in rural or remote areas. Community awareness of clinical training among interns might therefore have changed in recent years.
To investigate the associated geographic elements of the practice by interns, a nationwide survey was carried out in Japan to focus on the relationships between attitudes toward care provided by interns, and patients’ experience of this, and whether geographic and demographic variables affected acceptance or understanding of the need for intern training, especially following introduction of the new internship system.
Methods
Study design and participants
A nationwide survey was conducted using a representative sample of 2400 people (15–79 years) selected from the entire population of Japan in 2005. A custom research service (Nippon Research Center; http://www.nrc.co.jp/english/services/custom) was used and the inclusion criteria and sample size were fixed. Participants were selected by multistage stratified random sampling. Municipalities were selected, then specific areas within municipalities, and participants were then selected using the Japanese basic resident register. A total of 200 research assistants went door-to-door to conduct surveys with participants in March 2006. The research assistants visited each participant twice. During the initial visit, they asked participants to complete a paper questionnaire on their views on care from interns, plus demographic factors. They visited again to collect the questionnaire several days later. If the assistants could not contact the participants at the second visit, those people were considered to have declined to participate.
Questionnaire
The questionnaire was developed to measure the experience of and attitudes toward care provision by interns. Key questions addressed participants’ experience with, impressions of and requirements associated with treatment by interns. Most of the questions had multiple-choice responses. Eight non-medically trained people reviewed the questionnaire prior to the survey to improve its clarity and brevity.
Measurements and statistical analysis
Data were obtained on participants’ characteristics and opinions, including several on experience of and attitudes toward care provision by interns: experience of receiving care from an intern, willingness to accept care provided by interns and the reasons for this, and differences in acceptance of care from interns. Participants were also asked about the importance of nurturing the next generation of doctors and where interns should develop their clinical skills.
Anyone who had ever had a medical appointment with an intern, or whose family member had done so, was defined as having experienced care provided by an intern. Participants’ spouses, parents, grandparents, siblings, children and grandchildren were included as family members. Anyone answering ‘no/unsure’ was defined as having no experience of care provided by interns. Acceptance of care provision by interns was classified into binary variables. Participants who answered ‘I am indifferent about being seen by an intern’, ‘I want to be seen by an intern, if possible’, or ‘I would love to be seen by an intern’ were considered to accept care provided by interns. Those who answered ‘I absolutely do not want to be seen by an intern’ or ‘I do not want to be seen by an intern, if possible’ were considered not to accept care from interns.
To examine whether location influenced experience and attitude toward care provision by interns, participants were gathered from almost all regions in Japan and divided into five areas (Hokkaido and Tohoku, 15.4%; Kanto, 30.8%; Chubu and Hokuriku, 20.1%; Kinki, 13.6%; Chugoku, Shikoku and Kyushu, 20.0%). The participants were from communities with a variety of population sizes: 19.2% were from the 14 most populated cities, 30.9% from municipalities with a population of more than 150 000, 22.5% from municipalities with a population of 50 000–150 000, 8% from municipalities with a population of less than 50 000 and 19.3% from rural areas. Participants were classified into age groups: 15–19 years, 20–29 years, 30–39 years, 40–49 years, 50–59 years and more than 60 years.
People who had been treated by interns were asked for their impressions, and all participants were asked the reasons for their acceptance of care from interns, and for suggestions about interns’ clinical training. The data on geographic elements were analyzed against these responses.
Responses on the importance of nurturing the next generation of doctors were categorised as either ‘I should be willing or am willing to be examined by interns because nurturing doctors is very important’ or ‘I don’t want to be examined by interns, but I understand the importance of nurturing doctors’. Participants’ responses about where interns should train were categorised as either ‘only large tertiary hospitals’ or ‘smaller or community hospitals’.
All responses were coded as either binary or categorical variables. The details of both accepting and non-accepting participants were analyzed by grouping them based on their experience of receiving care from interns (experienced and inexperienced groups). Impressions about interns’ care provision among participants in the experienced group were classified as ‘accepting’ or ‘non-accepting’. Participants’ acceptance was also analyzed by participant past experience of having been treated by interns, their age group, the population of their municipality of residence, and region. The difference was assessed using χ² or Fisher’s exact tests. Statistical analyses were conducted using SPSS v20 (IBM; http://www.spss.com). Observations with missing data were eliminated from analyses and two-tailed p-values less than 0.05 were considered statistically significant.
Ethics approval
This study was approved by the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine (institutional review board number E160). Informed consent was obtained from each participant.
Results
Demographics
The sample data were representative of the Japanese population (128 million residents; mean age 43 years; 49% men (2005 census)). A total of 1109 (46%) participants completed the questionnaire. The gender ratio and mean age were consistent with the 2005 Japanese census (Table 1). In total, 10.2% (114/1109) of participants had received medical care from interns, of whom 4.5% (51 respondents) had direct experience. The other 5.7% (63) had experience of care provided by interns through a family member (indirect experience). Participants’ responses indicated that the situations most commonly involved hospitalization (60.5%), outpatient clinics (32.4%) or emergency room visits (5.2%).
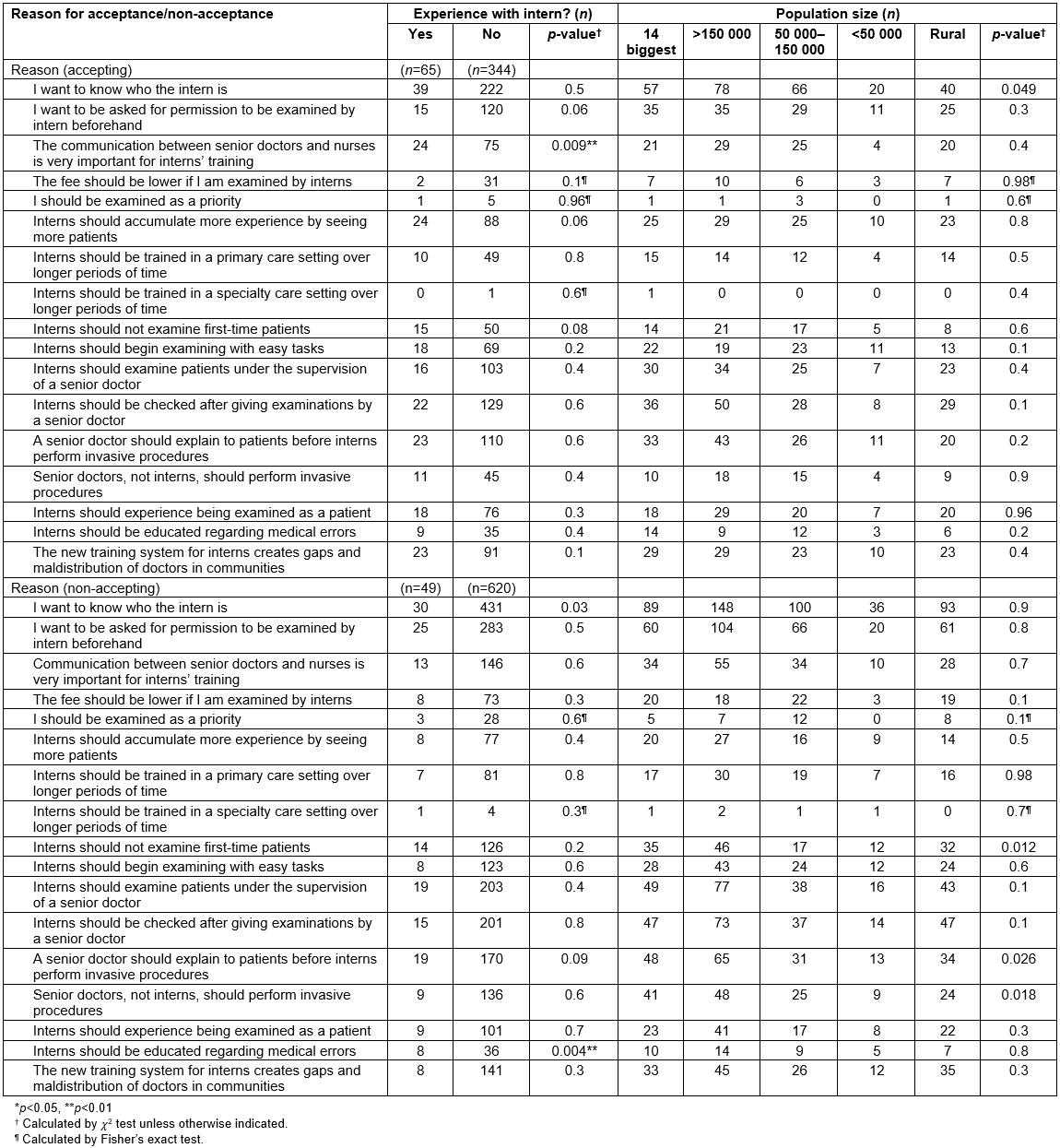
Table 1: Study participants’ characteristics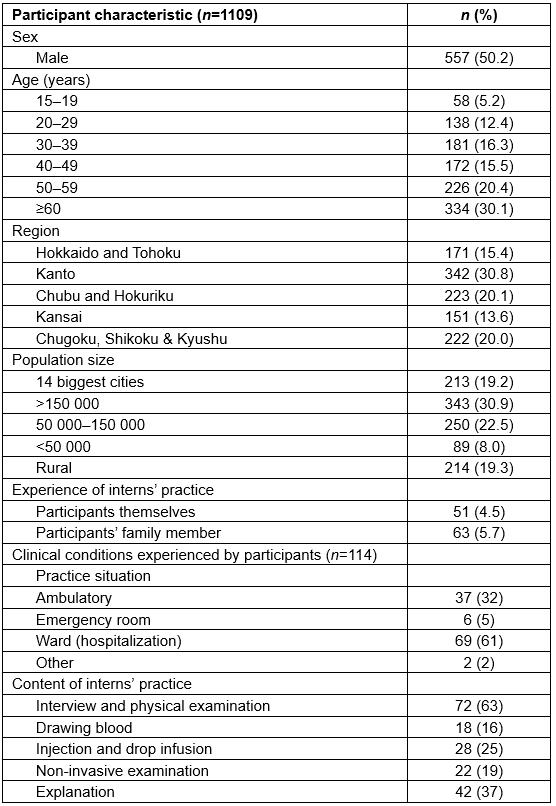
Attitudes toward care provision by interns
Overall, 37.0% (410/1109) of participants were comfortable receiving care from interns. Participants who had experience of care by interns were more likely to show acceptance than those with no experience (57% (65/114) vs 35.7% (344/964), p<0.001). Participants in larger cities were more likely to have experienced care by interns (p=0.04), but there was no significant difference by region (p=0.98). Neither population of municipality nor region was associated with satisfaction with care provision by interns (p=0.3 and p=0.5).
Acceptance of care provision by interns was not associated with region (p=0.8, Fig1a), population of municipality of residence (p=0.9, Fig1b) or age group (45.6%, 15–19 years; 43.4%, 20–29 years; 36.6%, 30–39 years; 38.2%, 40–49 years; 33.0%, 50–59 years; and 38.9%, ≥60 years; p=0.3). Those who were willing to accept care from interns were statistically more likely than others to express understanding that interns needed experience of providing care (accepting 91.6% (207/226) vs non-accepting 41.4% (143/345), p<0.001; experience 76.0% (57/75) vs no experience 59.3% (293/494), p=0.006). Participants who were willing to accept care from interns were also statistically more likely to respond that interns would have more opportunities to be trained at smaller or community hospitals than at tertiary hospitals (p<0.001, p=0.02, Fig2). This tendency was consistent across municipalities, regardless of population (57.5% for larger cities, 60.2% for municipalities with populations of over 150 000, 65.3% for municipalities with populations of 50 000–150 000, 57.1% for municipalities with populations <50 000, and 56.3% for rural areas; p=0.8). Satisfaction with care provision by interns was highest among those who had been seen in ward settings (73.9%, 51/69) and lowest in those who had been seen in an emergency room (33.3%, 2/6).
Table 2 shows reasons given by both those with experience and no experience of care provision by interns for accepting or not accepting care from interns, and the population of their home municipalities, stratified by acceptance. In total, 52% of accepting participants responded ‘because interns should have more experience’ and 29% responded ‘to further the advancement of medical science’. Among participants who would accept care provided by interns, those with experience of such care were significantly more likely to feel that interns were ‘polite’ (p<0.001) and ‘kind’ (p<0.001) than those with no experience with interns. The most common reason for non-acceptance was fear of negative aspects of care, particularly medical errors (p=0.03). There was no significant difference of acceptance among the population of the home municipality, the location of the community and any of the reasons for non-acceptance.
Table 3 shows the relationships among acceptance of care from interns, the population of the home municipality and the impressions of participants who had experienced care from interns. The following responses were significantly more common among those who accepted care provision by interns: ‘interns were polite’ (p<0.001), ‘interns’ practice was thorough’ (p<0.001), ‘interns worked very hard’ (p<0.001), ‘interns’ explanations were easy to understand’ (p<0.001), and ‘the intern seemed kind’ (p<0.001) Only one response, ‘the intern spent a lot of time’, was not positively associated with participant acceptance (p=0.3) but was associated with participants who lived in larger cities (p=0.02).
Participants with no experience of care from interns, but accepting of the concept, were more likely to respond that ‘communication between senior doctors and nurses is very important for interns’ training’ (p=0.009; supplementary table). Participants with no experience of and who were non-accepting of care provision by interns were more likely to respond that ‘interns should be educated regarding medical errors’ (p=0.004). There was an association between the population of home municipality and the response ‘I want to know who the intern is’ (p=0.049) among participants who would accept care provision by interns. This tendency was stronger in larger cities than in smaller municipalities. Non-accepting participants were also associated with the population of the home municipality for responses including ‘interns should not examine first-time patients because of the risk of misdiagnosis’ (p=0.01), ‘senior doctors, not interns, should perform invasive procedures’ (p=0.02) and ‘a senior doctor should explain to patients before interns perform invasive procedures’ (p=0.03). Those negative answers were more common in participants from larger cities than from smaller municipalities. There was no significant association between these demands and the region.
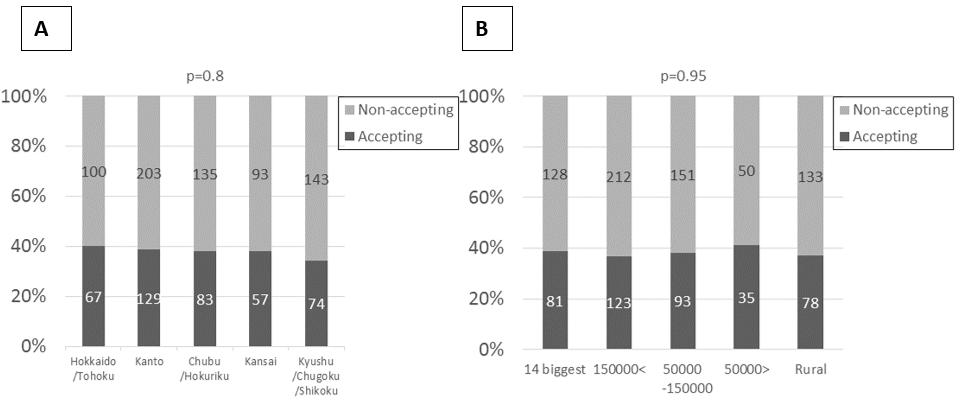 Figure 1: Acceptance of practice by interns in Japan by (a) region, (b) population of municipality.
Figure 1: Acceptance of practice by interns in Japan by (a) region, (b) population of municipality.
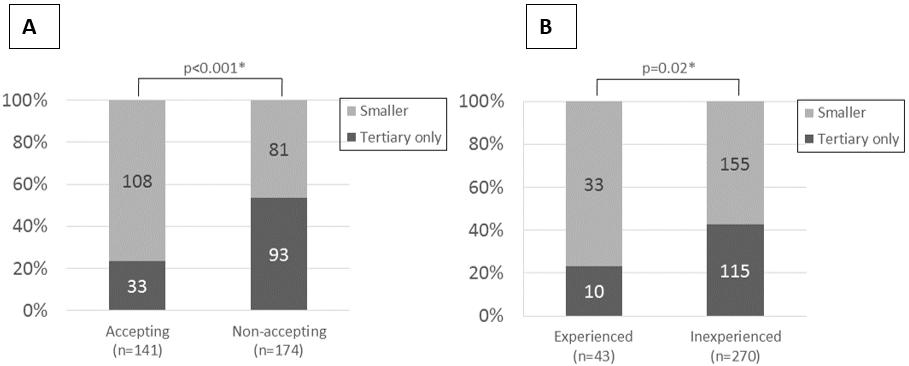 Figure 2: Perspectives of community residents on interns’ training site according to (a) acceptance/non-acceptance, (b) experience/lack of experience.
Figure 2: Perspectives of community residents on interns’ training site according to (a) acceptance/non-acceptance, (b) experience/lack of experience.
Table 2: Acceptance or non-acceptance of care provision by interns, by reason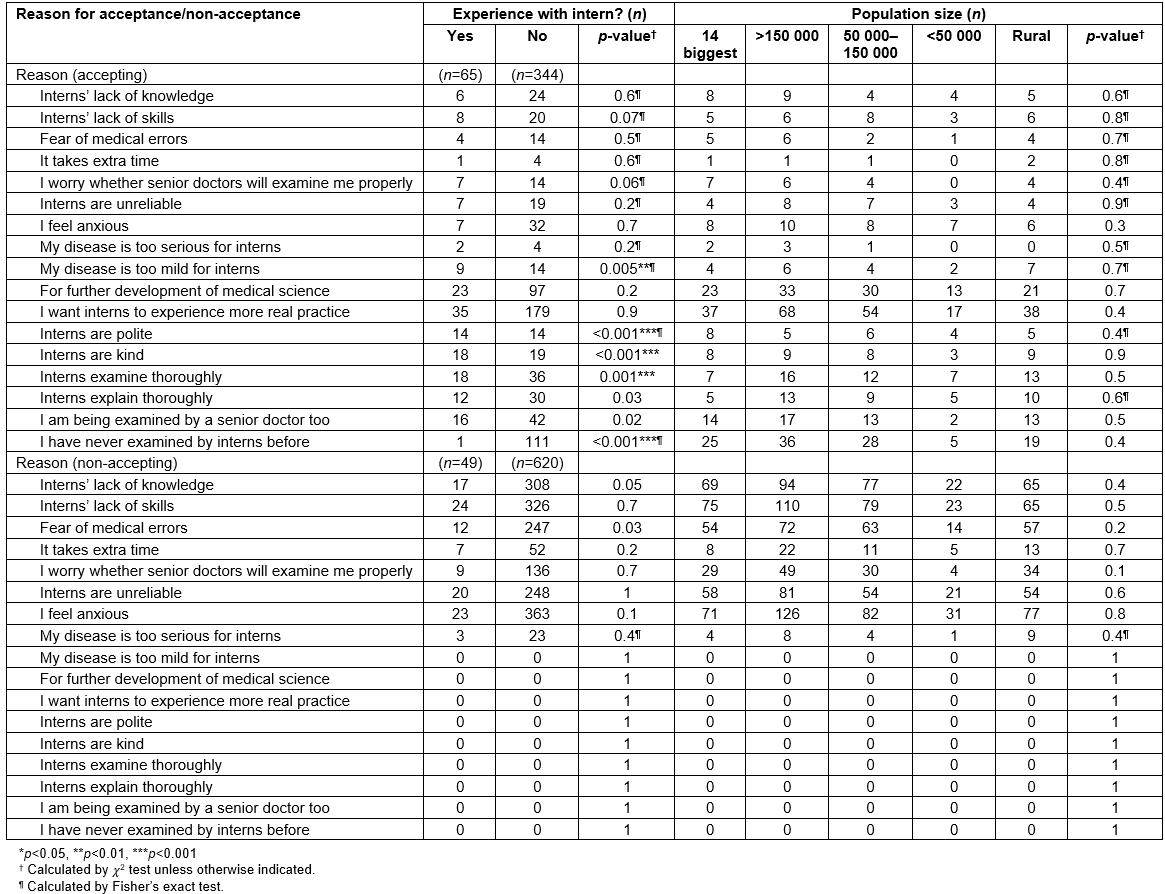
Table 3: Impressions of participants who have experience of care provided by interns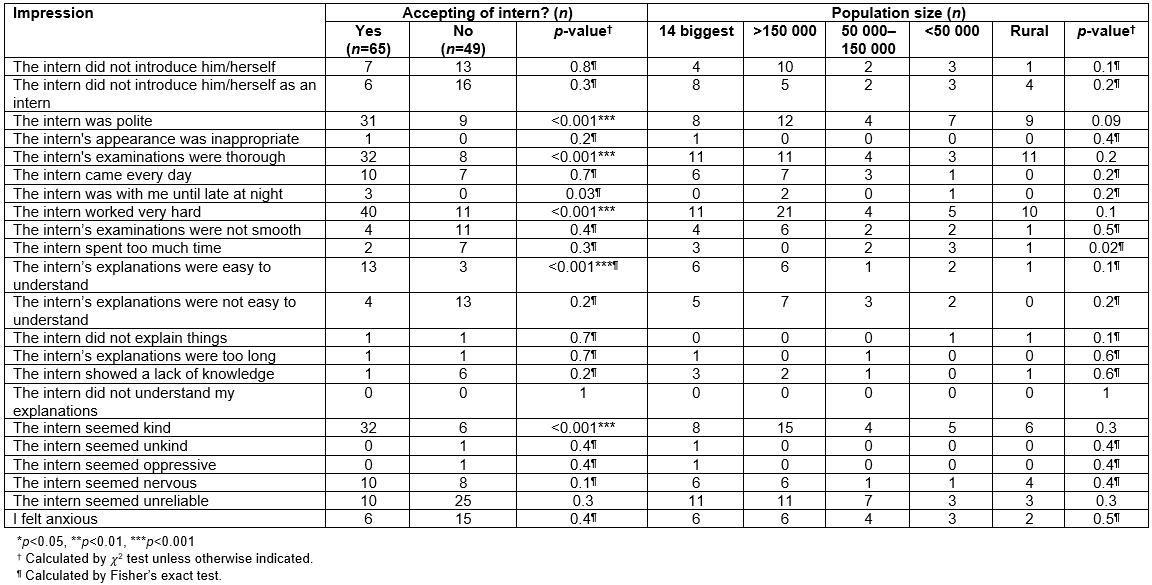
Discussion
Individuals’ experiences of and attitudes toward care provision by interns were analyzed by geographic and demographic variables following a nationwide survey. The analysis showed that people who had experienced or whose family members had experienced care provided by interns were more likely to accept care from interns than those without experience. Acceptance of care provision by interns was not associated with geographic variables such as region or population of municipality. Participants who accepted and had experienced care from interns tended to respond that interns should train at both tertiary hospitals and smaller and community hospitals. People who had experience of care provided by interns, either personally or through family members, and were accepting of this, responded that interns were generally ‘kind’, ‘polite’ and ‘thorough’. A few responses were associated with the population of the municipality of residence but, overall, geographic elements were not associated with the acceptance of care provision by interns.
In real-world settings, there are still sometimes difficulties in having interns examine patients, even when they have suitable qualifications1,2. It has been shown that patients participate in medical training largely out of altruism rather than obligation13,16. Several studies have shown that patients tend to accept treatment from medical students or interns when they are informed and give consent beforehand17. The significance of allowing interns to practice seemed to be understood by those participants who were prepared to accept medical care from interns. This suggests that dissemination of information about interns might be essential to improve patients’ acceptance of interns. Training hospitals and medical schools should disseminate information about practice by interns in several ways, and provide explanations to patients before obtaining informed consent. This might increase acceptance of care provision by interns. This research shows that, in smaller communities or hospitals, the dissemination task might be easier than expected.
As in previous studies, participants in this study who had already experienced care provision by interns were more likely to accept care from them in future18-20. This suggests that, as more people experience care provision by interns, the overall level of acceptance will grow. There is little evidence from previous studies of any relationship between patients’ acceptance of care provision by interns and geographic and demographic variables. There was a statistically significant association between the response ‘the intern spent too much time’ and participants who lived in larger cities, although this might vary with culture. The reason for this is still unknown but people in larger cities might tend to feel busy or feel interns are wasting their time if they take too long. If so, novice doctors might be able to take more time, and therefore benefit both themselves and the patients, in smaller cities. On most responses, the present study shows that variables such as region and population of the patients’ home municipality were not important factors in patients’ acceptance and overall attitudes. These results might show that the benefits of medical education in communities result from the training content or the size of community health facilities. Participants who reported having experienced care provided by interns were more likely to live in large cities than smaller municipalities. This might be because in Japan there are more training hospitals in large cities than in smaller municipalities. Participants who were prepared to accept and had experience of care provided by interns tended to respond that they believed it was important to allow interns to provide care because of their need for clinical education.
Patients who accepted care provision by interns tended to respond that interns should be trained in both large tertiary hospitals and smaller community hospitals. This is one of the most important results because it informs medical educators in communities that residents might prefer interns to have a wider range of experience. They might therefore be ready to accept interns as a part of the advancement of community-based medical education, as a clinical educational resource. There are many smaller hospitals in smaller communities in Japan, so the use of smaller community hospitals for clinical education is a reasonable option.
Patients appreciated characteristics of interns such as being ‘kind’, ‘polite’ and ‘thorough’. Interns’ bedside manner and attitude are very important in ensuring that patients are prepared to be treated by them. However, patients are anxious about whether interns’ clinical skill or knowledge is sufficient. To increase the rate of acceptance of care provision by interns, it might therefore be helpful to inform patients that, under Japanese law, interns only practice under the supervision of senior staff. In contrast to the results in this study, several previous studies have reported that patients accepted medical students’ or interns’ involvement15,21-24. There are multiple issues related to care provision by interns, so further research is needed to improve acceptance. Studies should examine views of patients, interns and instructors, and those of staff in hospitals, medical schools and governments. It may also be helpful to examine factors of cultural, historical and geographic diversity.
The present study’s findings should be interpreted in light of the study limitations. First, this study did not verify whether participants or their family members had actually experienced care provision by interns. Second, as these data were gathered only in Japan, the results may be influenced by unique cultural and social factors, including aspects of the medical system. These results therefore cannot be generalized to other cultural settings. In addition, the limited sample size and response rate might result in the statistically non-significant association between attitude and geographic variation. However, because a random sample of adult Japanese living in almost all areas of Japan was surveyed, these data provide a reliable and generalizable account of the Japanese healthcare setting. Finally, this study was a cross-sectional study, so the findings were primarily based on the correlations of observations. To attest these findings, more proactive methods to assess associations between acceptance of resident practice and geographical area should be considered.
Conclusions
This study provided a comprehensive picture of the geographic and demographic factors associated with patients’ attitudes toward care provision by interns in Japan. There were no significant differences in responses on clinical education by region, population of municipality or age group, which suggests that community-based medical education could be provided anywhere in Japan. Participants who accept and have experience of care provision by interns were more likely to respond that interns would be trained better at smaller community hospitals than at tertiary hospitals. Clinical education in Japan mainly takes place in tertiary hospitals at present, but this study suggests that further research into differences in acceptance level by hospital size or role may be helpful to clarify the benefit of community- and primary care-based medical education.
Acknowledgements
The authors thank Makiko Ohtorii and Ai Mizutani for their assistance with administration and data management. They also thank Melissa Leffler from Edanz Group for editing a draft of this manuscript.