Introduction
Heart disease has a high prevalence rate in Australia, affecting 30% of people over the age of 751. Annually, 700 000 presentations of myocardial infarctions (MIs) are seen within Australian emergency departments2. Based on high level evidence, percutaneous coronary intervention (PCI) is the recommended treatment option for coronary revascularisation following an MI3.
In an uncomplicated procedure the patient, post-PCI, is discharged home within 48 h and required to initiate behavioural changes and lifestyle modifications4,5. These behaviours include but are not limited to healthy dietary changes, increased cardiovascular activity, smoking cessation and medication adherence, all to prevent further cardiovascular disease (CVD)4,5. Referral and attendance to a cardiac rehabilitation (CR) program is recommended in light of the high level national and international evidence for the prevention of further risks associated with CVD3,6,7.
The National Heart Foundation Australia (NHFA) and Cardiac Society of Australia and New Zealand (CSANZ) guidelines recommend the focus shift from primary treatment to secondary prevention after a PCI is performed2. The goal of secondary prevention is to prevent further risks related to CVD, such as further morbidity or mortality. A repeat MI is avoided by strict medication adherence to prevent further plaque aggregation, along with actions to reduce the risk of comorbid conditions8. The Australian Cardiovascular Health and Rehabilitation Association identifies the secondary prevention measures of smoking cessation, reduction in weight and cholesterol, healthy eating, building on cardiovascular endurance and adherence to prescribed medications as imperative to preventing CVD8. The importance of early secondary prevention has been corroborated by both the European Society of Cardiology Acute Coronary Syndrome (ACS) guidelines outlined by Steg et al7, and the American Heart Association PCI guidelines9. Moreover, the latter guidelines state that dual antiplatelet therapy (DAPT) is prescribed for a minimum of 12 months following insertion of a coronary stent9. The aforementioned guidelines are required for CVD risk reduction and must be adhered to following a PCI8,9.
Patients in rural populations are 1.3 times more likely to die from ACS compared to urban city dwellers10. There are several hypotheses for these health inequalities, such as resistance to behavioural changes, and reduced access to healthcare services for follow-up care11-13. Rural populations account for 30% of Australian residents14, meaning 30% of Australians have reduced access to resources. Furthermore, rural and regional Australians experience generally poorer health than metropolitan inhabitants, making them at higher risk for ACS and other cardiovascular conditions8.
Secondary prevention has proven to be an effective strategy for patients with ACS post-PCI15,16. Lifestyle modifications and behavioural changes, such as healthy dietary intake, physical activity, smoking cessation and medication adherence, are suboptimal within Australia. It remains unknown which secondary prevention measures are being undertaken and maintained by this group of rural Australians, as there is limited available evidence. Therefore, this review aims to systematically map current literature on rural Australian health behaviours following a PCI.
Methods
Research design
A systematic scoping review was undertaken. Scoping reviews gather multiple study designs as a way to collect and synthesise information, identifying gaps in literature and guiding future research initiatives17,18. A scoping review was chosen to map out the existing literature without bias, and to discover concepts relating to the rural Australian cardiac population. The Arksey and O’Malley19 and Armstrong et al20 methodological frameworks were implemented, consisting of five stages: research question identification, identification of studies, selection of studies, charting the data, and summarisation and discussion of the results.
Search strategy
The literature was systematically reviewed in January 2018, using six electronic search databases: Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed Central, Embase, ProQuest and PsycINFO. Search strings were applied using medical subject headings, relevant synonyms and Boolean operators. The following main search topics were adapted to each of the databases: ‘behaviours’, ‘rural’ and ‘PCI’. One operator screened the studies along with reference management software. Additional publications were discovered by manually searching bibliographies from relevant articles. The search was limited to English publications within the 2007–2017 timeframe. The selected timeframe was to ascertain that influence of high level post-PCI evidence on health practices. Earlier literature was excluded to ensure recent trends in health practices and behaviours were collected. Australia has a higher obesity rate when compared to the global average 27.9% compared to 19.4%21. Australians also score one of the lowest smoking rates 12.4% compared to the global average of 18.4%21. Therefore, searches were limited to Australian research studies to ensure relevancy to the unique population. ACS is managed both medically and surgically; however, it is possible to undergo a PCI without having ACS22. The goal of this search was a wide scope of literature, and thus ‘PCI’ was the term searched rather than ‘ACS’.
Inclusion criteria
Given this review aim, publications that involved the rural Australian cohort during the post-PCI period were included.
Data extraction
Articles were indexed within a table format for extraction of key literature components (Table 1). Categories of lead author, study design, location, population under study and interventions were displayed for primary analysis. Data were also extracted in relation to the research aim, and overall key results (Table 1).
Table 1: Studies included in scoping review, with key findings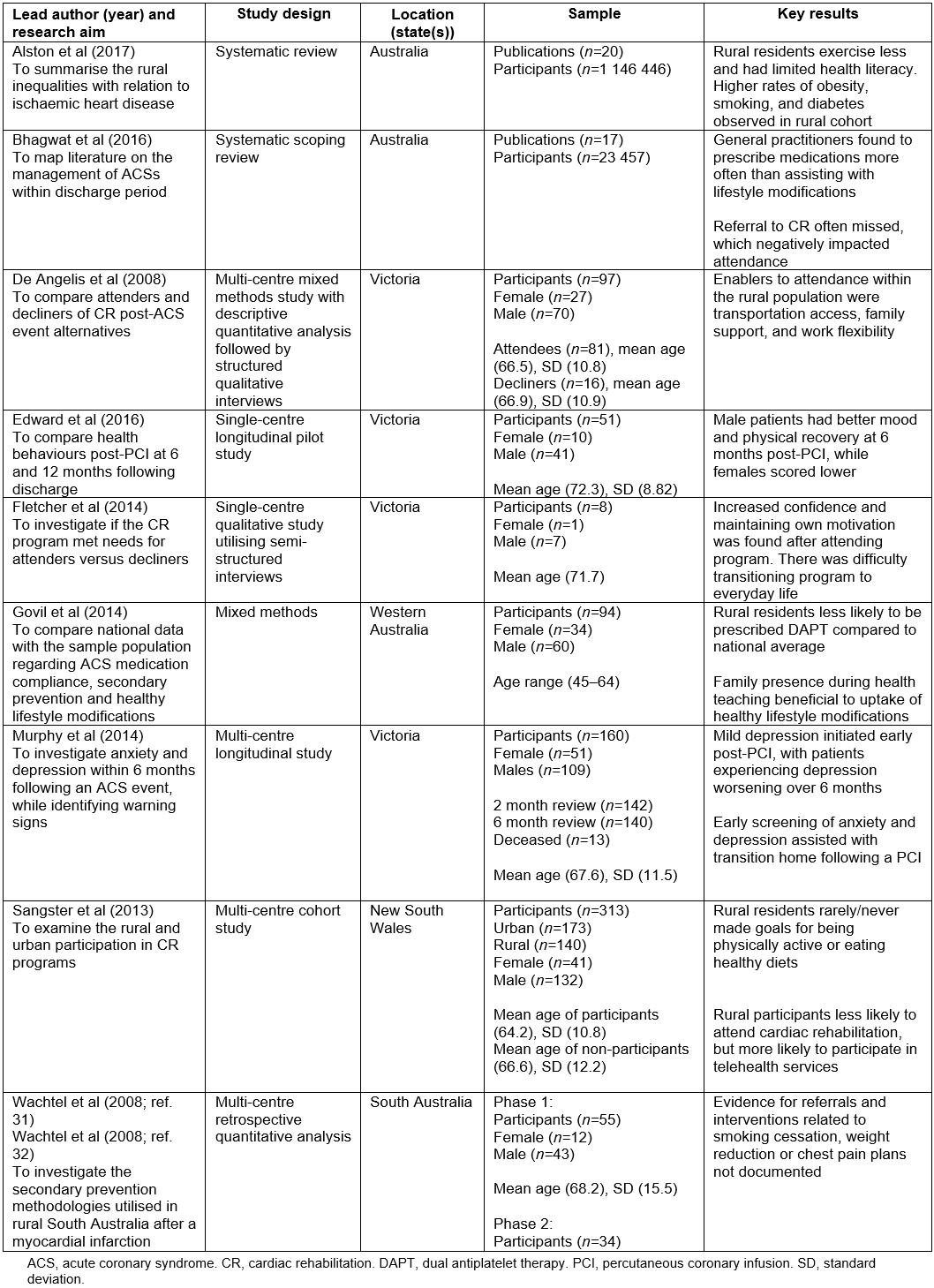
Results
A total of 1480 citations were retrieved, with an additional 13 articles obtained by a manual search. Ten articles met the inclusion criteria for this scoping review (Fig1). Research studies had varied methodologies: quantitative (n=4), qualitative design (n=1); mixed method (n=2) and two systematic reviews. Two articles reported the findings of the same study (Table 1).
Five studies assessed ACS discharge behaviours over time, including interventions from the primary care perspective. CR and reasons for patient compliance, attendance, and the comparison of rural and metropolitan residents, were reported within three publications. Two publications outlined a comparison of patient demographics pertaining to CVD and ACS within the rural and metropolitan regions of Australia (Table 1).
Three common themes from the studies’ findings were identified: poor attendance at CR programs, psychosocial stress and isolation, and difficulty transitioning to healthy lifestyles.
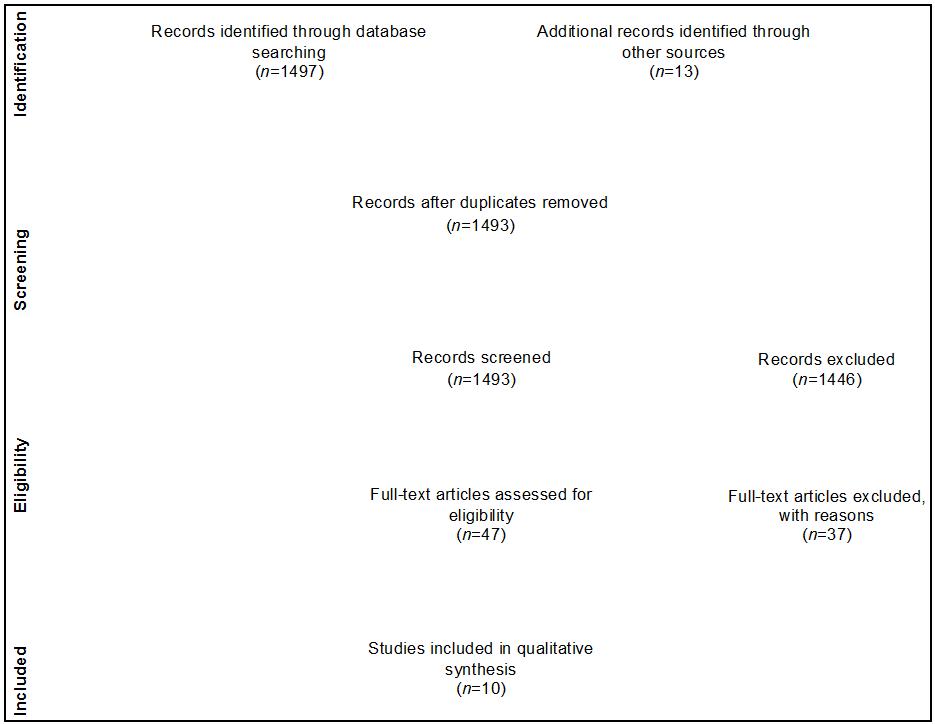 Figure 1: Scoping review PRISMA flowchart23.
Figure 1: Scoping review PRISMA flowchart23.
Referral to and attendance at cardiac rehabilitation
Four studies highlighted the poor CR attendance rate among rural Australian residents24-27. Sangster et al discovered 60% of their rural and 45% of the urban cohort did not attend a CR program24. De Angelis et al found 16% of their sample population failed to attend a rural CR program25. Those who declined CR highlighted travel expenses as barriers to attending a program25. Attenders of CR lived a mean of 15.4 km from a CR program, whereas decliners of the CR program lived a mean of 40.4 km in distance25. Sangster et al found that 73% of patients who lived over 100 km or more from a facility declined attending a CR program24. Sangster et al also found 48.6% of urban and 51.4% of rural participants declined CR24. Younger residents, with a mean age 64.2 years compared to 66.6 years, were more likely (p<0.001) to engage in telephone-operated CR programs and were more likely to be from a rural rather than urban location24.
An enabler to attending CR was the support and referral from GP or hospitals upon discharge25. A scoping review by Bhagwat et al found that attendance rates of CR were heavily influenced by referral rates at time of discharge26. Rural residents most likely to be referred to a CR were those who were married and younger in age26. Govil et al sampled members of the Aboriginal community in rural Western Australia diagnosed with CAD and found a preference for closer proximity to medical services and identified other factors for poor attendance such as issues with child care and other family obligations27.
Isolation
Seven publications documented issues of abandonment by healthcare professionals or lack of social supports25,27-32. De Angelis et al found the participants believed there was minimal time allocated to psychological concerns during CR25. Edward et al indicated that, at six months post-PCI, women were more likely to be depressed, with a perception of reduced social support28. The lack of support for members of the rural cardiac cohort was also identified to be an indicator for anxiety and depression during the post-discharge period, with 29% of residents having worsening depressive symptoms29. Fletcher et al found rural residents felt alone, isolated, abandoned by healthcare professionals and received minimal follow-up care once integrated back into the community after discharge30. Moreover, unmarried rural participants highlighted the difficulties of poor social support in the postoperative period30. The importance of the family within the education period was also identified as a factor for patient behaviours27. Despite the evidence that social supports correlate with healthy lifestyle behaviours, Sangster et al found, within their sample of 140 rural residents, that only around 4.9 participants received social support for healthy diets, and 4.1 residents had support for becoming physically active24.
Wachtel et al discovered similar results when auditing rural post-ACS medical records, whereby 11% of patients in hospital and 29% in the GP clinics were referred to rehabilitative health services31. One rural community identified poor communication by medical professionals at time of hospital discharge27 and were less likely to receive management plans and support services in comparison to the national average.
Transitioning difficulties
Eight publications documented that rural patients had difficulty with successfully transitioning back into the community with healthy lifestyle changes24-28,30,31,33. Living rurally was not linked to increased mortality rate at 30 days post-cardiac revascularisation; however, Alston et al found the survival rate was worse at 7 years post-PCI33. The rural attitude is one of being self-sufficient, getting on with life without asking for assistance, and resistance to lifestyle changes was clearly a factor for those who declined CR25. Fletcher et al found that rural residents were hesitant to exercise outside of the CR program; however, high levels of supervision gave residents more confidence30.
Fletcher et al highlight behaviour change (ie diet and medication adherence) as a difficulty for their sample population30. Participants of the CR program were instructed on ways to exercise, how to prepare healthy meals, and overall self-management of ACS30. Despite what is learned in CR, the health risk profiles studied by Sangster et al identified poor diets high in white bread were being consumed more by rural rather than urban residents with CAD, despite being prescribed healthy cardiac diets24. Sangster et al also discovered 50.7% of rural residents underutilised strategies, such as setting goals and collaborating with GPs, to manage their health, compared to 32% of urban residents24. Bhagwat et al identified residents in multiple rural communities engaging in poor behavioural and lifestyle choices, such as smoking post-MI26. Additionally, Govil et al found rural residents to be non-adherent to medications, only consuming them when feeling unwell, and experiencing difficulty undertaking lifestyle modification27.
Discussion
Guidelines from the NHFA and CSANZ recommend secondary prevention strategies post-PCI, and rural residents are evidenced not to meet these criteria. The distance to CR programs has clinical significance during referral and attendance, and rural residents are less likely to attend. The postoperative period is a critical time, and the inclusion of a support system to reduce depressive symptoms is beneficial, but rural residents report feeling isolated. Poor communication was multifactorial during the discharge period, which led to confusion and misunderstanding, further isolating the rural residents. Only 12 months post-PCI, the rural population was engaging in unhealthy lifestyle choices, such as smoking, unhealthy diets and physical inactivity. Rural residents rarely set their own goals, accounting for a poor 7-year survival rate among rural residents diagnosed with CVD.
Travel is a large barrier faced by the rural residents of Australia, indicating that those in the most remote regions have minimal access to CR services in comparison to the metropolitan residents25. Rural residents were more likely to decline attending a CR program if they had to travel over 15 km24,25. Proximity must be taken into account when choosing an appropriate CR method of delivery to ensure equality and likelihood of attendance24. Additionally, travel costs (eg petrol) to the CR program was a barrier25. Socioeconomic disadvantage was present in the majority of rural residents residing in NSW compared to their urban counterparts24. A reduced income and earning potential explains the aversion to attending a CR program with the increased cost of petrol. The telephone-operated CR program was a strategy investigated to overcome the barrier of reduced CR attendance and the younger rural cohort participated in these telephone services, which indicates a future potential for telehealth to bridge this gap for the technologically adept residents.
Indigenous Australian people living with cardiac disease found child care and other family obligations were major barriers for participating in CR27. Geographical isolation is a major barrier to attending CR in Australia34. This phenomenon was also observed in a survey conducted by Shanmugasegaram et al among rural Canadian inhabitants13. Clinicians have initiated strategies to mitigate these geographical challenges, such as remote teleconferencing CR sessions and outreach programs35. Local cardiac outreach programs have developed to provide an alternative to secondary prevention services closer to home36. Outreach programs are advantageous for bridging the gap for access to CR, goal-setting and reducing the feelings of isolation36. However, the program is similar to CR and is futile without proper referral from acute hospitals, along with hesitation and non-participation by individuals36. Rural Indigenous Australian populations may benefit from a telephone CR program, as this will allow participants to stay at home tending to social and family obligations, and still benefit from the services.
The discharge time is pivotal for rural Australians, and referral to a program prior to discharge provides them with a higher engagement level8,25,26. Referral to CR provides patients post-PCI with support and services to facilitate their recovery37. The relevance to these findings could mean the restructuring of the discharge period in hospital to ensure rural residents are receiving referrals to the program prior to leaving the facilities. Surprisingly, younger, married rural residents were more likely to receive referral to a CR program, for unknown reasons.
The design of the CR program does not allow for a lengthy discussion of psychological issues with facilitators and other members25. The strength of the CR program has been to find commonality and support among members of the community who have experienced similar physical and mental hardships30. Rural residents have felt the barrier of isolation when they have not been provided opportunities to heal on a spiritual level25,30. Holder et al recommended an appointment with a spiritual counsellor to help patients during the recovery process following an ACS event38.
Within 6 months of discharge post-PCI, Edward et al28 found women to be generally depressed, highlighting women required further social supports28,29. The specific factors contributing to this disparity have not been identified; however, Murphy et al identified higher risk of depression among rural unmarried Australians29. Suggestions to overcome this healthcare issue are cited as multiple screenings, congruent with Australian guidelines for inpatient risk assessment for anxiety and depression29. The CR program is designed to include spouses during sessions, in efforts to mitigate isolation25. Unmarried and single rural residents identified feelings of isolation and hardship within the postoperative period27,30.
Rural residents felt minimal assistance from health professionals when integrating back into the community30. Similarly, in New Zealand, Beasley and Dixon found the transition from hospital to community CR was sometimes overlooked within the rural population of New Zealand, necessitating further interventions during this period11. Rural Australians had indicated they were discharged without a scheduled follow-up appointment, were not given a point of contact and did not receive chest pain management plans27 or cardiologist referral31. These concerns are clinically significant and represent abandonment and neglect by healthcare professionals.
The rural Indigenous Australians identified abandonment by health professionals as an issue27. Cultural barriers such as institutional racism, misunderstandings, fear and poor health literacy are factors leading to this disproportion39. Considerations need to be taken around the history, health inequalities, social determinants of Indigenous health, and the impacts on medication adherence in a secondary prevention space. Aboriginal populations are more likely to discharge from hospital against medical advice, prior to learning about secondary prevention strategies, contributing to higher rates of morbidity and mortality12,39. Participants in this study indicated they could not understand the medical terminology, and health professionals did not measure their level of health literacy27. These findings may indicate health professionals have not prioritised postoperative health education and teaching, or health literacy was overlooked in the provision of post-PCI education, therefore leading to increased anxiety and feelings of isolation in the rural cohort. The implementation of Indigenous health workers is one strategy utilised to overcome this barrier39. Indigenous health workers are particularly advantageous in the hospital setting because they have an intimate cultural awareness and sensitivity. Indigenous health workers have access to services within communities, bridge health terminology barriers and work to reduce risks of discharging against medical advice12,39. To ensure a successful transition, education and teaching sessions tailored to the level of health literacy, along with cultural competency training and safety frameworks, may be required.
A meta-synthesis by Brundisini et al systematically analysed rural access to healthcare services from Europe, Australia, New Zealand and North America40. The authors found a culture of self-reliance and avoidance of remote health care as a commonality among the rural populations. Patients living rurally were less likely to attend urban clinics and hospitals for fear of being an outsider, a theme termed ‘rural attitude’ also discovered within this scoping review25,40. The rural attitude characteristics include a stubborn persona, resistance to healthy lifestyle modifications and difficulty with insight into one’s own illness25. Communication for the rural community needs to be succinct and action plans in place, prior to discharge41. Breaking down this barrier is imperative to recovery for the rural residents exhibiting these patterned behaviours. The NHFA and CSANZ recommends patients post-PCI adopt physically active lifestyles during their recovery period to adhere to secondary prevention guidelines3. Conversely, it was discovered 12% of rural patients have ceased exercise at 1 year26. Australia shares similar transitioning difficulties to other developed countries, as evidenced by a Canadian study by Pesut et al42. This study concluded the rural Canadian demographic also experienced barriers to committing to lifestyle changes, such as lack of transportation to CR and issues with accessibility for healthy dietary choices.
Medications prescribed following a PCI, such as DAPT, must be taken daily to effectively prevent platelet aggregation and in-stent stenosis9. Rural residents were only taking medication when symptomatic, highlighting that this population did not understand the properties of DAPT therapy27. A randomised controlled trial by Rinfret et al evaluated if telephone calls from nurses had an effect on medication adherence43. Results concluded 43% of patients post-PCI in the control group were not adhering to the prescribed DAPT whereas 87% of patients in the intervention group did self-administer DAPT when receiving telephone contact by nurses43. On the contrary, Cheng et al argue that patients’ post-PCI suffer depression, which contributes to medication non-compliance, particularly with DAPT44. Regardless of the contributing factors, medication non-compliance is a dangerous risk, associated with rehospitalisation and a high mortality rate45. It is the responsibility of all health professionals to ensure the properties of DAPT are understood and demonstrated by patients41,45. These measures will allow for a more successful transition back into the community, reducing the risk for a repeat hospitalisation.
A treatment gap is evident, where rural residents are engaging in unhealthy lifestyles, which is increasing their risk of rehospitalisation, morbidity and mortality. Future research might aim to review strategies for reducing costs associated with travel to a metropolitan CR program, such as the induction of the telephone-based CR program, and uptake of outreach programs34. Reasons for the older generation refusing telephone-based CR are not fully understood and present a gap in the literature. The aforementioned isolation concerns have been recognised as a gap within care provided by the Australian healthcare system. Further research is required to audit national trends of care provided at time of hospital discharge for post-PCI rural residents, to ensure NHFA and CSANZ ACS guidelines are being met. During CR, healthy activity is promoted, including strategies to incorporate exercise into daily living going forward; however, it remains unknown why rural Australians cease undertaking physical activity, despite early interventions, thus highlighting a gap in research, necessitating an area for future investigation. Whether a majority of rural residents have reverted to unhealthy habits, or never fully transitioned, is unknown..
Strengths and limitations
Conclusions from the systematic review conducted by Alston et al indicated that minimal studies have delved into the inequalities and ACS disparities within the rural Australian groups33. However, this scoping review was able to focus on the health behaviours of rural Australians, making a unique contribution to postoperative cardiac care. Utilising a variety of search databases strengthened this scoping review. Presenting this research in the form of a scoping review created several benefits. Inclusion of studies with different methodologies allowed for greater insight into the phenomena and multiple gaps were identified within the literature by utilising a systematic mapping technique, and thus identification of areas for future research.
Despite the multiple strengths reported, this scoping review had limitations. Search parameters excluded rural populations residing outside Australia, but there may be a stronger link to international commonalities than originally hypothesised. The rural population may be largely underrepresented due to the lack of available literature, especially given that 30% of Australian residents live in rural locations and two-thirds of Aboriginal and Torres Strait Islanders reside in rural Australia, a group also identified as having greater rates of morbidity post-cardiac event12,39. Long-term evidence relating to the benefits of CR has not been thoroughly reviewed, and further research would be required to determine the long-term effects on factors such as morbidity and mortality.
Conclusions
Secondary prevention for CVD post-PCI is highly recommended for all residents of Australia. This review aimed to determine the available literature surrounding the health behaviours of post-PCI rural residents. Rural Australians have lower CR attendance rates compared to urban residents, and report feelings of isolation and abandonment by family and healthcare professionals. Additionally, it was discovered that rural Australians did not make successful transition to adopting healthy lifestyles, re-engaging in unhealthy behaviours. The future health care of the rural population would benefit greatly with additional research, analysing compounding factors and identifying further specific treatment needs.




