Introduction
The population is ageing at an increased pace, and it is now predicted that people aged 60 years or older (ie elderly) will outnumber the children aged less than 5 years in the near future. Around 80% of these older people are expected to be living in low- and middle-income countries by the middle of this century1. In recent years, India has focussed on strengthening the health system to support healthy ageing through the National Programme for Health Care of the Elderly (NPHCE)2,3. While in the Indian context, health of the elderly largely remains a problem of access and affordability nested in the context of complex social dynamics, the exacting burden of non-communicable diseases including lifestyle diseases and disabilities thereof should not be undermined3,4. The geriatric population is vulnerable, as they mostly exhibit poor healthcare seeking behavior, ultimately leading to poor quality of life and avoidable death1. The tribal areas, being marginalized and practicing their own indigenous customs, facing the challenge of accessibility and affordability of health care, require special consideration while dealing with issues affecting the health of the elderly.
Fall is one of the important factors leading to what is now termed as ‘geriatric syndrome’1. Around 10% of these fall victims require medical care5. In recent years, there has been an increase in published researches focussing on falls among the elderly in India6-12. Despite this impetus, only few studies have approached the issue in a longitudinal manner, and attempts to find out factors behind recurrence of the episodes of injurious falls is a rarity. Some studies have focussed on the rural community, but the elderly population from tribal areas was not studied6,8,10. According to current knowledge, this topic is less studied in the Indian context, and research on this issue is lacking in the eastern part of India. Doing the study in a tribal population is unique because they are the vulnerable population, and lack of data makes it difficult to formulate an informed policy framework. Earlier studies conducted in different socio-economic contexts revealed several risk factors associated with recurrent fall-related injuries such as age, sex, physical inactivity, living situation, psychosomatic conditions, sensory and mobility-related issues. But whether and to what extent these factors are applicable for the tribal elderly has not been explored, and an estimate of the magnitude of the issue among this underprivileged population is not available.
When discussing health of the geriatric population, prevention of injurious falls is a very important cost-effective strategy6,13. In the same continuum, recurrent injurious falls, if prevented, will result in effective reduction of social and economic stress. Fall episodes can be prevented by active intervention after identifying the risk factors. A longitudinal design of study yields evidence of temporality in the relationship of risk factors with occurrence of falls. By identifying such key intervention areas of health promotion to prevent recurrent falls, the evidence from this study will aid policymakers to improve the relevant health programs to a more robust level. The current study therefore aimed to find out the incidence of injurious falls among elderly participants from tribal areas of West Bengal, India. It also measured the effects of selected predictors on recurrent injurious falls among this population.
Methods
Study design and participants
A prospective observational study was conducted in 16 tribal dominated villages under two selected community development blocks of North 24-Parganas district14-16,West Bengal, India from December 2017 to January 2019. Home-dwelling elderly participants (aged ≥ 60 years), who were residing permanently (≥10 years) in a selected village and living with at least an adult person, were included in the study after obtaining written informed consent for participation. Only ambulatory elderly individuals were selected. However, those with diagnosed cardiometabolic or musculoskeletal diseases, cognitive impairments, or neurological or psychiatric diseases were excluded. Those having bony fracture or associated diseases attributed to non-fall events were also excluded. After recruitment the participants were followed up for 1 year through four quarterly contacts. A minimum of one follow-up at the third month was considered mandatory for inclusion in the final analysis.
Sampling and recruitment
Participants were selected from the villages using probability proportional to size technique. The sample size was calculated using the power cox program in Stata v14.2 software (StataCorp LLC, https://www.stata.com/stata14)17,18. At 95% level of confidence and 90% power, taking the average detectable hazard ratio to be 0.25, 20% attrition and 30% prevalence of recurrence, the estimated sample size was 25410,13. Adjusting for a design effect of 2, the sample size was estimated at 508. Inflating for an estimated partial- or non-response of 10%, the target sample size was 559. A total of 548 participants were recruited in the study. The scheme of the study is presented in Figure 1.
Table 1: Baseline characteristics of participants according to follow-up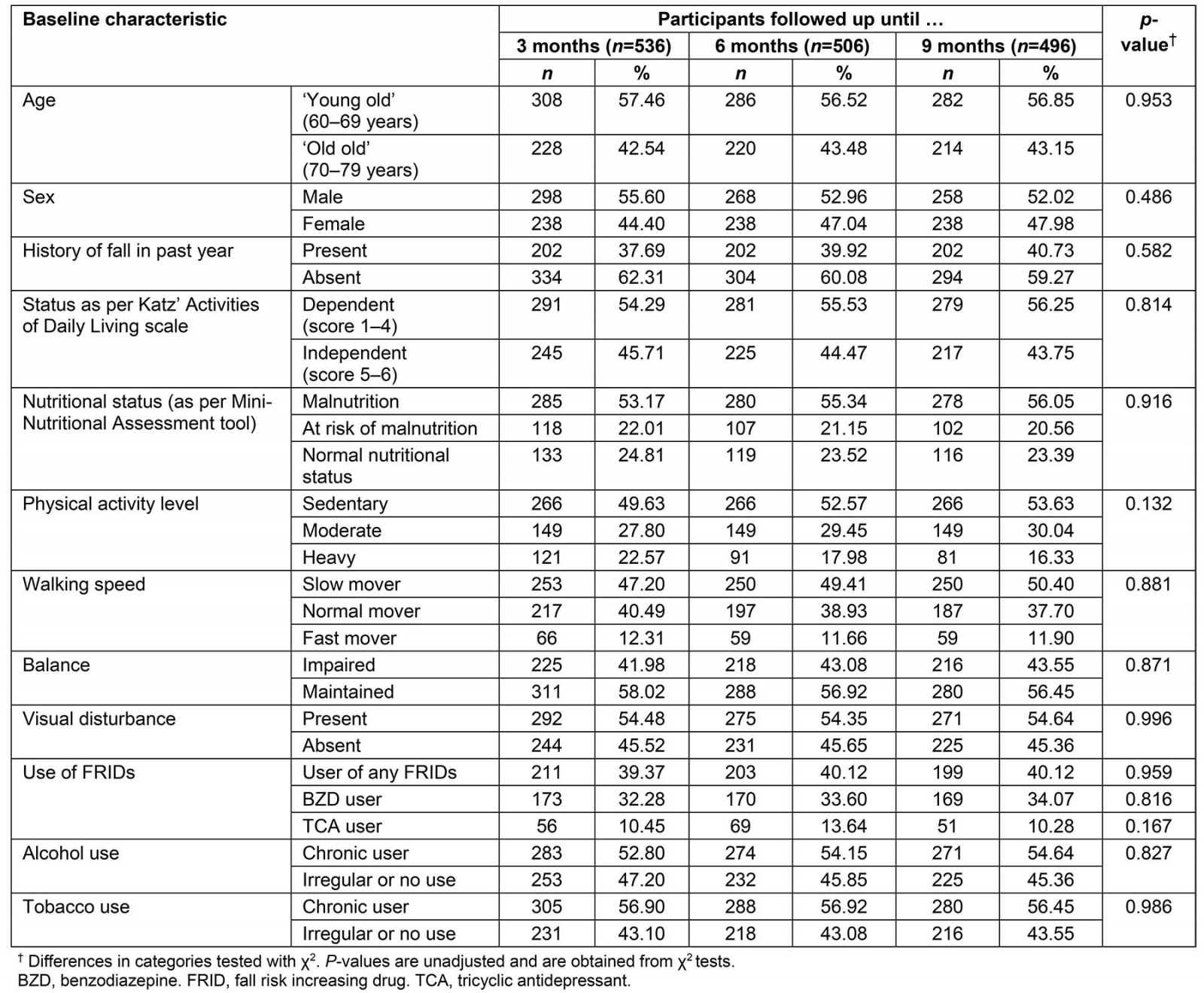
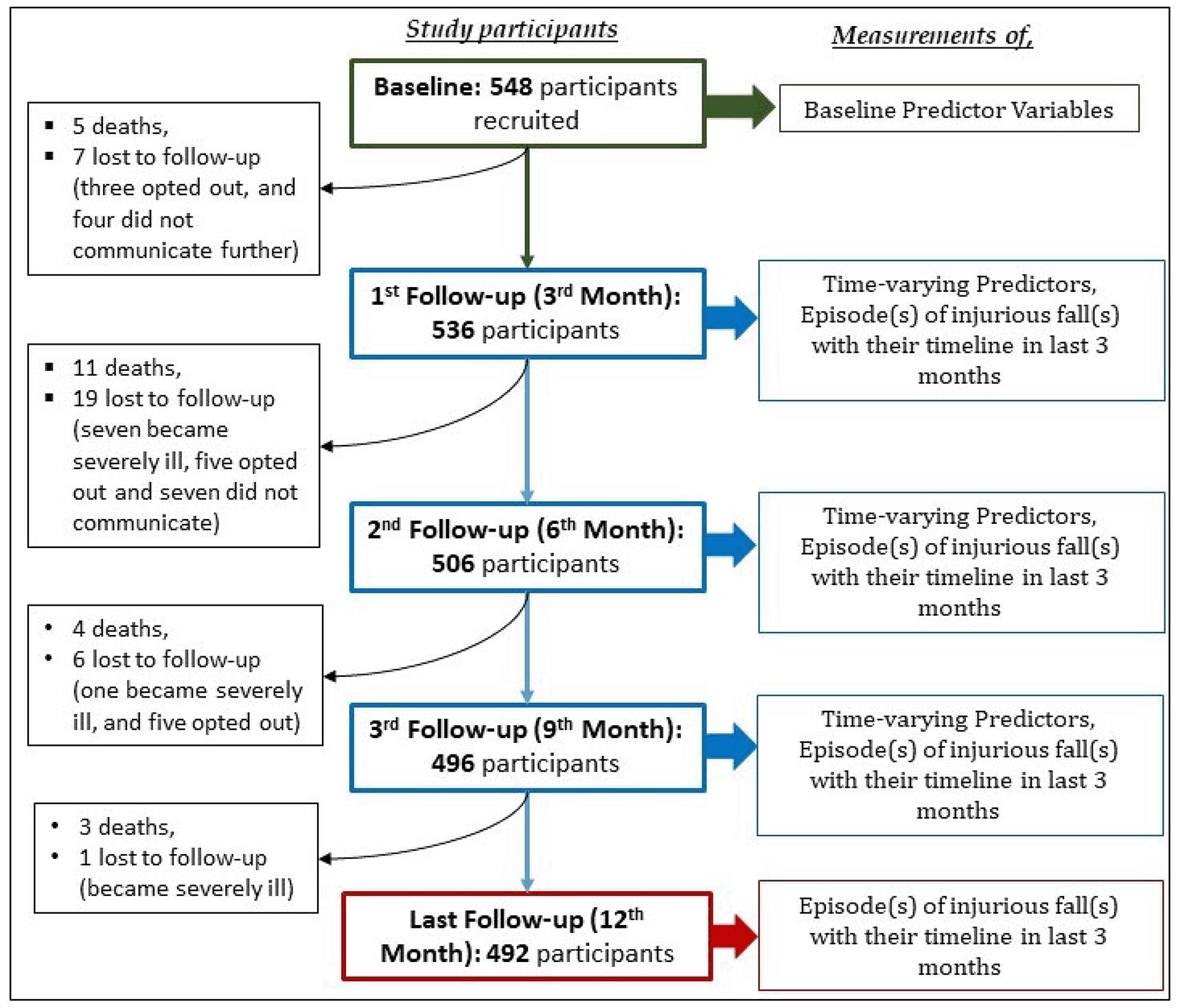 Figure 1: Scheme of recruitment participants and follow-ups.
Figure 1: Scheme of recruitment participants and follow-ups.
Study variables and data collection
Interview for data collection was done with the help of a pre-designed, pre-tested schedule. After recruitment and baseline data collection, follow-ups were done at the completion of the third, sixth, ninth and twelfth months. The variables measured during these follow-ups are shown in Figure 1. Sociodemographic information (eg age, gender, religion, type of family and level of education) were self-reported by the respondent with or without aid of a caregiver. Use of alcohol and tobacco products were considered. Those who currently used any tobacco product were considered current users of tobacco19. Use of alcohol was categorized as ‘chronic users’ (at least one drink per week over past one year) or ‘irregular or non-users’13. Physical activity was categorized as sedentary, moderate or vigorous based on daily activities of the respondents20.
The nutritional status of the elderly participants was screened with the help of the Mini Nutritional Assessment – Short Form (MNA-SF) tool. The MNA-SF tool classified the respondents into normal nutrition, at risk of malnutrition and malnutrition, based on dietary history, history of involuntary weight loss, mobility, psychological stress, neuropsychological problems and body mass index21-23. Independence in performing daily activities was assessed by the Katz index of independence in Activities of Daily Living (ADL) scale. The ADL scale considers bathing, dressing, toileting, transferring, continence and feeding as the basic activities and notes dependence in each activity, yielding a highest score of 6, which implies independence24,25. Data regarding use of fall-risk-increasing drugs (FRIDs) including psychotropic medication were collected from each respondent and triangulated with the response of their caregiver26,27. Balance was measured by testing the ability to stand on one leg13,28,29. Walking speed was classified into ‘fast movers’, ‘normal movers’ and ‘slow movers’ according to standard measurements13. Self-reported visual disturbance, being a validated measure, was also noted30.
Injurious fall was defined as an episode of fall leading to bodily injury and receiving professional medical care31. History of injurious fall in the past year was elicited from each participant and/or the caregiver at the time of recruitment. Episodes of injurious falls and durations of hospital stays, if any, during the study period were noted during subsequent follow-up visits. Occurrence of more than one episode of fall for the same individual during the follow-up period was considered as a recurrent fall.
Statistical analysis
The data collected were entered online in real-time mode during follow-up visits using predesigned Google forms. The entered data were available for analysis through automatically generated Google sheets. Statistical analysis was done using Stata v14.2. Participants were categorized into two age groups: 60–69 years (‘young old’), and 70–79 years (‘old old’)32. Those scoring 4 or less in ADL were considered dependent. When modelling recurrent falls, physical activity levels of moderate and vigorous were classed as non-sedentary, while slow and normal walking speed were combined into a ‘slower’ category.
The outcome (recurrent injurious falls) had two components: time until occurrence of the first fall and effect of different predictors on recurrent falls. Due to the recurrent nature of the event, the population at risk at the beginning of each quarter were those completing follow-up in the previous quarter, irrespective of their status of sustaining a fall. Therefore, the survival time analysis for time until an episode was done separately for each quarter. It was conceptualized that not only an episode of injury has an effect on a subsequent event, but also the time of hospitalization, if any, following injury served as a time gap during the period of follow-up. Therefore, effects of the fall predictor variables were assessed using the Prentice, Williams and Peterson Gap Time (PWP-GT) model, considering the Cox proportional hazard model was inappropriate to model recurrent events33-36. The regression model was developed with history of a fall in the previous year, age at recruitment and gender as time-independent variables. Nutritional status, dependence, physical activity, use of FRIDs, visual disturbance, addiction status (alcohol and tobacco), balance and walking speed were time-varying variables (variables interacting with the follow-up time). The effects of the predictors were reported in terms of adjusted hazard ratio (aHR) and its 95% confidence interval (95%CI). P-value <0.05 was considered statistically significant.
Ethics approval
Ethics clearance was obtained from the institutional ethics committee of Medical College and Hospital, Kolkata (ref. no. MC/Kol/IEC/Non-Spon/569/05-2017). Written informed consent was obtained from the participants while recruiting in the study. No incentive was provided to the participating families.
Results
Baseline information of study participants
Among the total recruited participants, 536 geriatric participants who completed a follow-up after 3 months post-recruitment were included for analysis. A total of 506 participants were followed up until 6 months and of them 496 were followed up until 9 months and 489 until 12 months (ie 1 year of observation). The baseline characteristics of the study participants and along the phases of follow-up are shown in Table 1. The mean age of the participants at the start of follow-up period was 69.16 (±2.95) years, with the eldest participant aged 78 years. The majority (57.46%) were ‘young old’ (60–69 years) at the time of recruitment. Around 55.60% were male and 49.63% had a sedentary level of physical activity. It was observed that most of the participants were Hindu, belonging to Scheduled Tribes, currently married and residing in a joint family. Most of the participants were chronic users of alcohol and tobacco products. Around 37.69% had a history of injurious fall in the preceding year. At the time of recruitment, 53.17% had malnutrition according to the MNA-SF tool. At the sixth month (ie second follow-up) the proportion of malnutrition was 55.34% because a higher proportion of participants with normal nutritional status were lost to follow-up. A similar trend led to a malnourished proportion of 56.05% at the third follow-up (ninth month). According to Katz’ ADL scale, the mean score was 3.75 (±1.99). More than half of the participants (54.29%) were dependent on caregivers for ADL. Although 47.20% had a slow walking speed, 58.02% did not have impairment of balance. Visual disturbance was reported by 54.48% participants. Use of psychotropic medications was not found to be a prevalent practice.
Episodes of injurious falls
During the 1-year follow-up period there were 153 reported episodes of injurious falls in the study group. No individuals suffered more than one episode of injurious fall during any follow-up quarter. Figure 2A depicts the proportion of individuals reporting an episode, while Figure 2B shows the proportion of episodes in each quarter of follow-up. The highest proportion of individuals suffering injurious falls was reported during the first 3 months (9.51%), while the next 3 months (3.73%) had the lowest reported proportion. Out of the total episodes of fall, 33.33% occurred during the first 3 months, and in the subsequent quarters the proportions were 13.07%, 29.41% and 24.18% respectively. Excluding the days of hospitalization following an episode, the incidence of fall calculated was 29.88 episodes per 100 person-years.
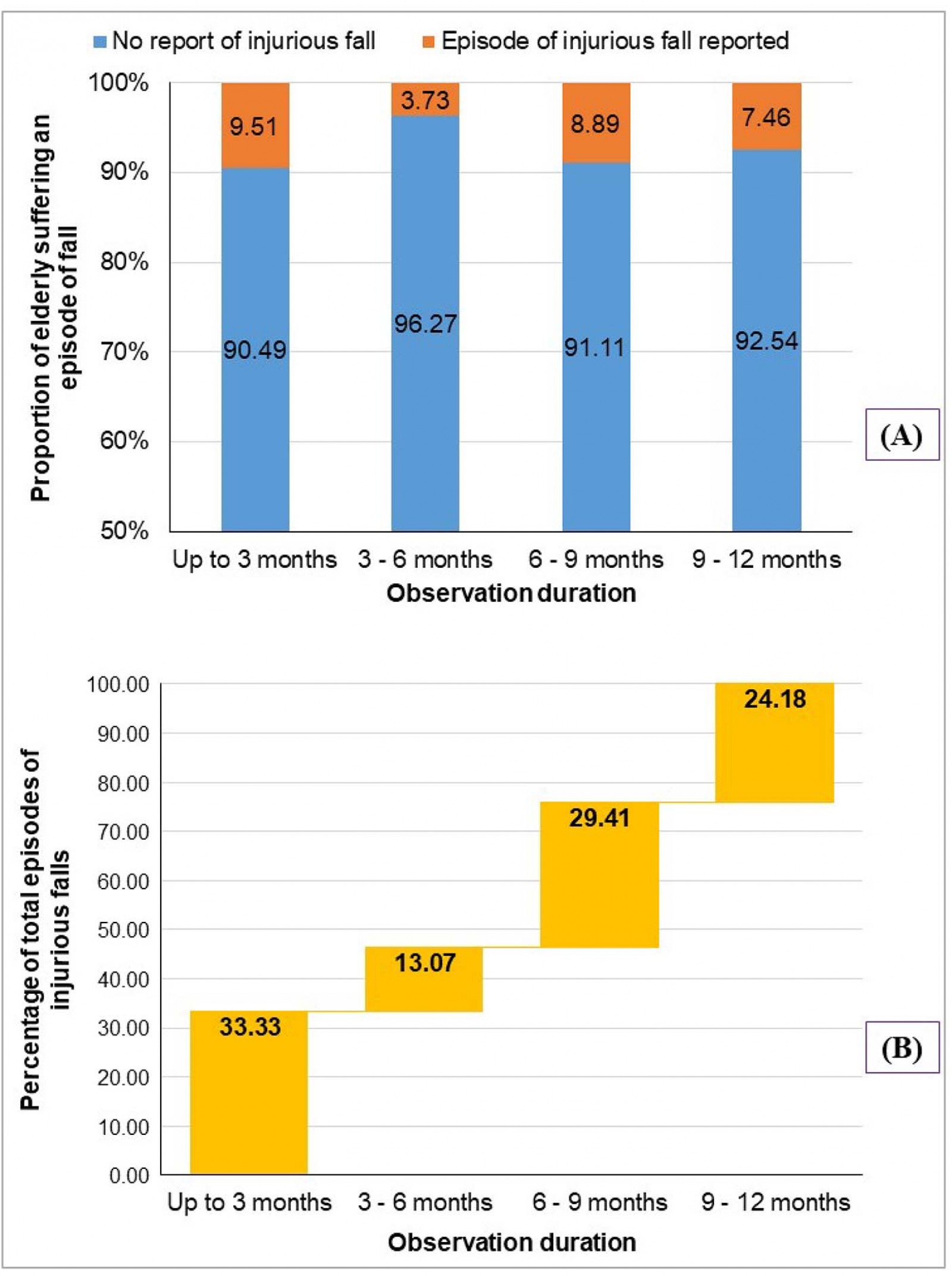 Figure 2: Episodes of injurious falls as per observation quarter. (A) Proportion of elderly individuals reporting episodes of injurious falls; (B) Proportion of quarterly injurious falls out of total reported episodes of falls.
Figure 2: Episodes of injurious falls as per observation quarter. (A) Proportion of elderly individuals reporting episodes of injurious falls; (B) Proportion of quarterly injurious falls out of total reported episodes of falls.
Predictors of injurious fall
Figure 3 represents the survival curves for sustaining an episode of injurious fall during each quarter. In the first 3 months the mean duration for occurrence of an episode was 2.85 (95%CI: 2.81–2.89) months. For those who were followed until 6 months, the mean duration of sustaining a fall in the second quarter of follow-up was 5.96 (95%CI: 5.94–5.98) months. For those followed up until 9 months and 12 months, the mean durations of sustaining an episode in the third and fourth quarters were 8.85 (95%CI: 8.80–8.89) and 11.89 (95%CI: 11.85–11.93).
The predictors of recurrent fall among the geriatric study participants are shown in Table 2. Having a history of fall in the previous year at the time of recruitment was found to have a 133% higher chance of sustaining recurrent episodes of injurious fall (aHR: 2.33; 95%CI: 1.01–5.38). When adjusted for time, compared to normal nutritional status those at risk of malnutrition had a 53% higher chance (aHR: 1.53; 95%CI: 2.54–9.23) and those having malnutrition had a 20% higher chance (aHR: 1.20; 95%CI: 1.01–3.60) of suffering recurrent falls. Those having an impaired balance had a hazard ratio of 5.96 (95%CI: 3.52–6.34) as compared to those maintained balance. The hazard ratio observed for a faster walking speed was 3.23 (95%CI: 2.12–5.26). The effects of use of psychoactive medication, physical activity or addiction were not found to be statistically significant. Although visual disturbance showed a 13% higher chance of sustaining recurrent falls, this effect was not statistically significant. While considering the effect of dependency, it was observed that the dependent elderly had 99% less chance of sustaining recurrent injurious falls (aHR: 0.01; 95%CI: 0.00–0.03), implying dependency regarding daily living activities to be a protective factor.
Table 2: Predictors of recurrent injurious fall among study participants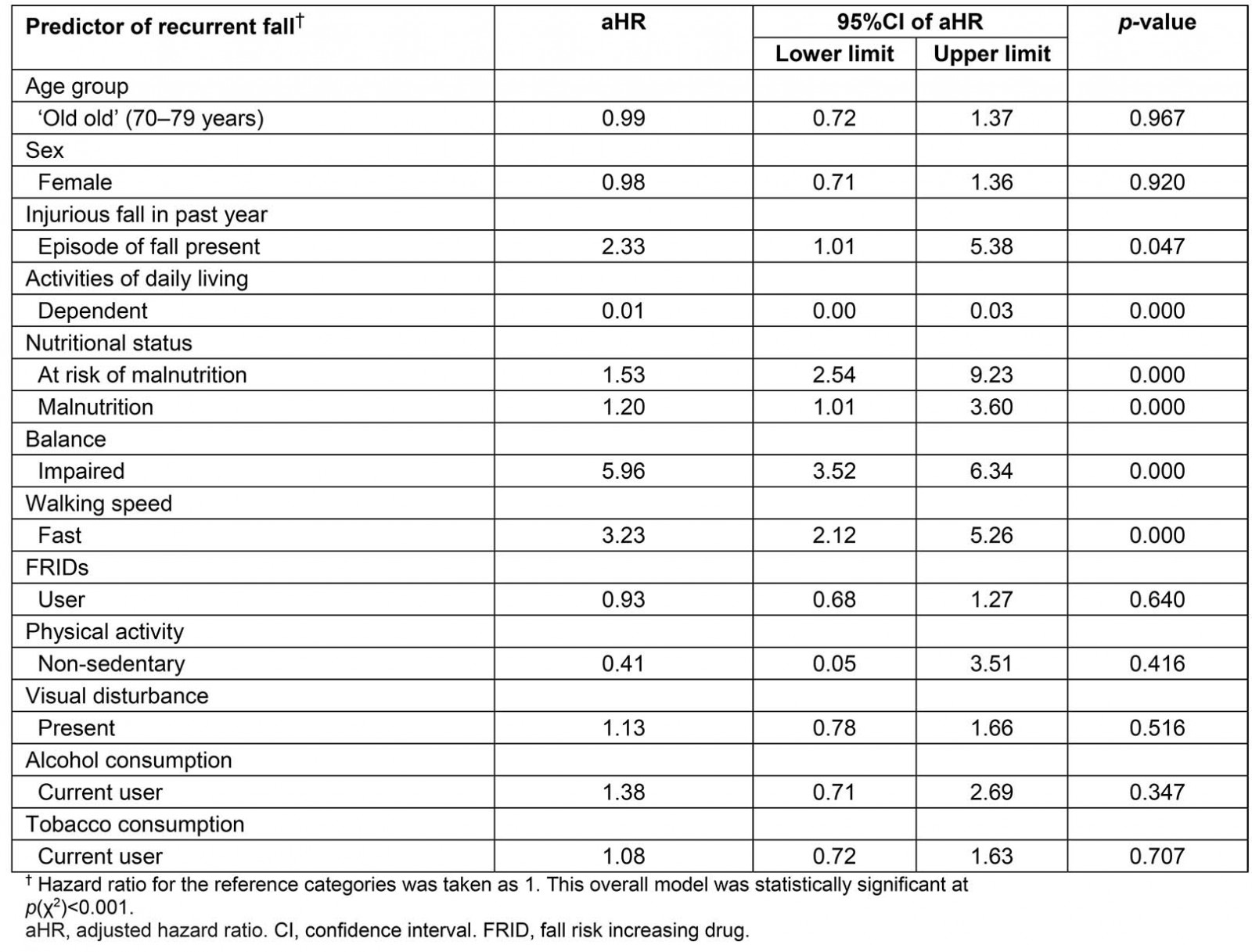
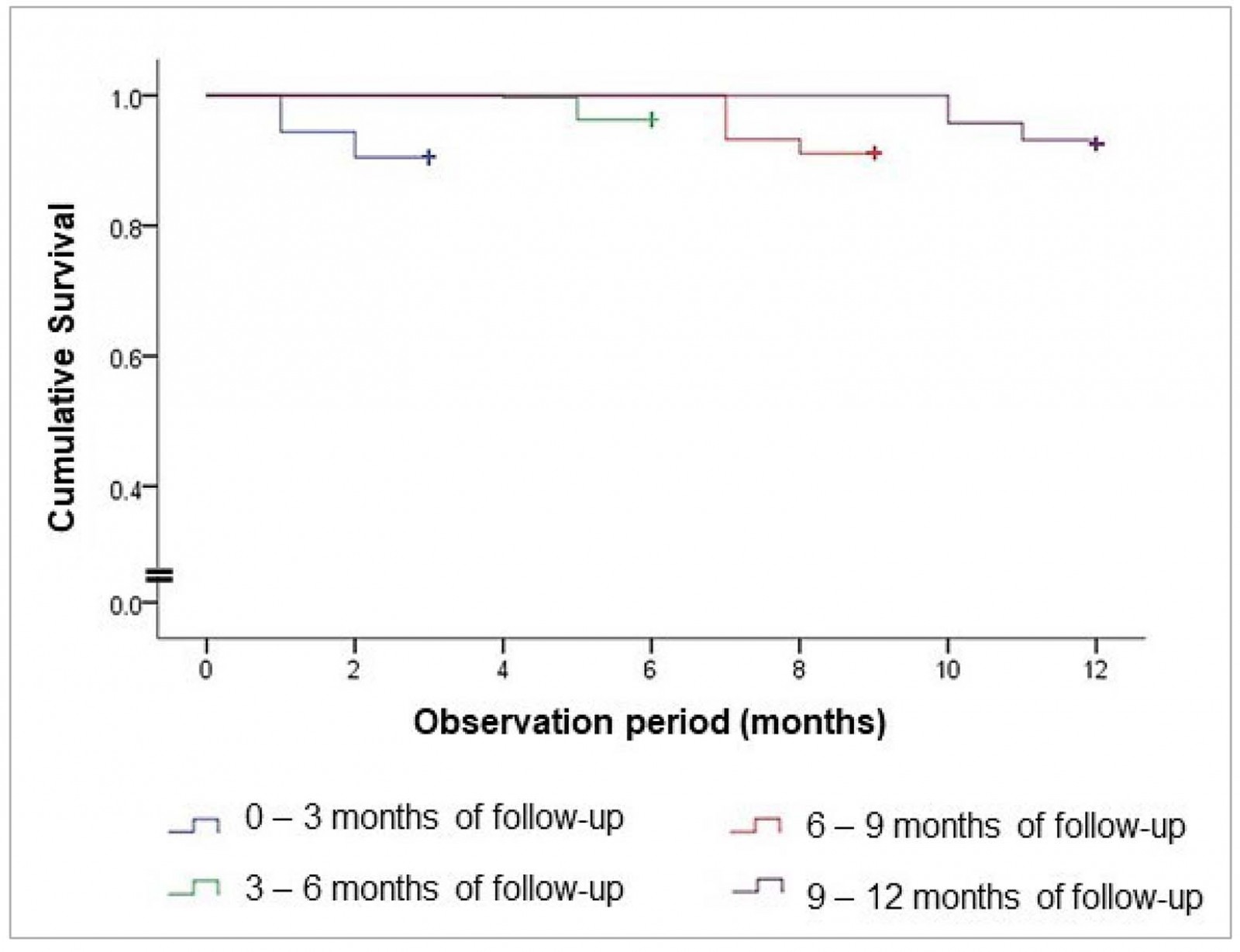 Figure 3: Survival curve for incidence of injurious fall per observation period.
Figure 3: Survival curve for incidence of injurious fall per observation period.
Discussion
Findings in light of previous literature
The current article reports a 29.88 per 100 person-years incidence for an episode of injurious fall among the elderly. This is comparable to the prevalence of around 20–30% reported in several studies5,10,13,37. A previous fall was found to put an elderly individual at risk of an injurious recurrence. In their cross-sectional study, Chacko et al reported age to be a significant correlate of falls10. But in the present study the effect of age was not statistically significant. This may be due to the fact that the age range of the studied population was less dispersed.
Sirohi et al, in their cross-sectional survey in rural Haryana in India, demonstrated functional disability and visual impairment as significant correlates of falls6. However, the present study showed visual impairment to be a risk factor for recurrent falls, but dependency (functional disability) to be a protective factor. The effect of visual impairment was, however, not statistically significant. A possible explanation could be that dependency restricts mobility of the elderly, and the dependent elder is most of the time aided by a caregiver, reducing the probability of sustaining injury. The tribal communities are known to take care of their elders. It may be a factor in dependent individuals being protected from the risk of recurrent falls. Visual impairment, on the other hand, acted as a probable confounder in view of dependence. This explains visual impairment not being statistically significant with dependency as a predictor. The effects of addictions, physical activity and use of FRIDs were not significant statistically. This can be reasoned by their interactions amongst themselves and with the other significant predictor variables.
Most of the cross-sectional surveys report prevalence of fall to be significantly higher among women6,7,10. However, in the present article the hazard of incurring recurrent fall was statistically not significant for women. The present study included participants who lived with at least one caregiver. Also, the majority of the participants belonged to a joint family. These imply the participants were expected to receive better social and family support, explaining the contrasting finding. Nutritional abnormality, balance impairment, gait disorder and addiction habits were found to be important correlates of falls as per another cross-sectional study from south India7. In consonance, the present study established abnormal nutritional status, impaired balance and faster walking speed to be risk factors for recurrent falls. But effect of physical activity was not found to be statistically significant. In the present study, more than half of the participants were found to be malnourished. Such a high burden of malnutrition itself requires a separate thrust. Those having poor nutritional status were at substantial risk of sustaining injurious fall episodes recurrently.
Strengths and limitations
The majority of the studies dealing with the correlates of falls in the elderly in an Indian context have considered comorbidities as the chief contributors8,10. However, in the present research, several of the comorbidities were set as exclusion criteria, allowing the study of the biophysiological effect of different factors itself. But the current study did not screen the participants continuously to identify and exclude several cardiometabolic morbidities during the course of the study, due to logistic constraints. This is a limitation to the study despite the rigorous attempts to exclude participants with diagnosed morbidities. The importance of considering injurious falls over simple fall events is in minimizing the recall bias associated with reporting of events of interest. Moreover, from a clinical and public health point of view it is important to prevent injuries. Considering the design and analytical technique used in this study, perhaps it is one of the few studies in the Indian context measuring the risk of recurrence of injurious falls, using a statistically robust method. The use of the PWP-GT model accounts for the alteration in risk when hospitalized, thus providing a more accurate estimate of risk situations for recurrent falls among the elderly when residing in the community. While most studies report the prevalence of falls, the current article reports the incidence, by virtue of its longitudinal design.
Implications of findings
The high burden of malnutrition provides actionable evidence from a public health point of view for rigorous nutritional improvement programs for the disadvantaged elderly. The effect of addiction habits on recurrent falls was not significant statistically. However, the proportions of chronic alcohol or tobacco users were around 50–60%. This warrants serious behavior change communication, as the ill-effects of such prevalent addiction practices extend beyond episodes of fall-related injuries. The study recommends that the revealed risk factors, particularly prevalence of elderly malnutrition, lack of awareness and attitude regarding healthy dietary practices, high alcohol and tobacco addiction, lack of health care and rehabilitative facilities to address the balance or gait problems, should be adequately addressed while developing the program for health care for the elderly in India. There is strong advocacy of developing a separate program focussing on nutrition of the elderly, and development of a de-addiction framework. Along with the clinical care made available, the NPHCE may require assistance with these components, or maybe a merged approach is required. The proportions of fallers were higher during the first and third quarter of follow-up. This can be conceptually correlated with the abundance of rainfall during these periods, resulting in accidental falls often leading to serious injuries. Therefore, an environmental effect requires further in-depth assessment.
Conclusion
Intensive care to those having a history of an episode of fall is probably the best way to prevent recurrence. Provision of proper nutrition, by means of economic development, ease of accessibility and awareness generation regarding healthy dietary practices, is an important cornerstone in prevention of recurrent injurious falls. Although addiction did not have any significant effect, the proportion of alcohol and tobacco use was found to be high in the tribal-dominated villages studied. Measures should be taken to curb these behavioral factors. Regular check-up and rehabilitative measures to aid individuals with balance or gait problems are also required. Moreover, a positive and constructive attitude should be garnered to improve the health of the elderly, especially in marginalised or disadvantaged populations, which will propel the community one step closer to attaining healthy ageing. The findings advocate for an interdisciplinary approach in assessing and mitigating the risk factors of recurrent episodes of injurious fall.
Acknowledgements
The authors acknowledge the study participants and their caregivers; without their support the study would not have been possible. The local non-governmental organizations and the members of the Panchayati Raj Institutions extended their support during data collection for the study.



