Introduction
The current outbreak of COVID-19 disease has led to rapid and widespread changes to practice1. The primary care response in Scotland has involved the development of coronavirus assessment centres open 24 hours a day and staffed by general practitioners (GPs), nurses and support staff including drivers, domestic staff, nursing assistants and administrators2. Patients with symptoms of COVID-19 are asked to call a centralised triage service, which then passes on the case to the coronavirus assessment centre if further assessment is required.
Significant emphasis is placed on avoiding direct patient contact, by using both telephone and video consulting. Should any further investigations such as pulse oximetry be required, novel approaches such as testing while a patient is still in their car can be considered.
This case demonstrates the processes used to enable a paediatric patient residing in a remote community with suspected COVID-19 disease to have her mother speak with a GP in the coronavirus assessment centre, have investigations performed in her own home to rule out pathological arrhythmia and obtain prompt advice from a geographically distant specialist.
Case report
In 2020, the mother of a girl aged 5 years called the 111 non-emergency medical advice phone line regarding her unwell child. The family live in a rural area of a remote Scottish island group with a total population of less than 30 000.
She spoke initially to a call handler who collected demographic data, and her call was then transferred to the triage GP, who took a medical history over the phone. Both were based in Inverness, more than 160 km from the patient. The mother described the child as having being unwell with a cough for 2–3 weeks, which had worsened in the past week, during which the child developed a concurrent fever and green nasal discharge. The fever was recorded between 37.9ºC and 38.2ºC and was described as being present continuously for 5 days before settling and recurring intermittently since. No clear focus of infection was noted – specifically, no rash, urinary symptoms, eye involvement or gastrointestinal disturbance. She had no dizziness or episodes of syncope.
The child was described as being quieter and less energetic than usual, spending more time on the couch; however, she still had a good appetite and at times seemed energetic and more like her usual self.
The child’s mother was a healthcare professional and had noted an irregular pulse when checking for tachycardia. She also identified a normal respiratory rate of 26 breaths/min, a pulse rate of 94 beats/min and temperature of 37.8ºC.
The call was triaged as requiring further assessment due to the persistent fever and potential arrhythmia, so it was referred to the coronavirus assessment centre. The GP there had a further telephone consultation with the patient’s mother and thought the child may have had a COVID-19 infection but was unsure how to manage any arrhythmia.
Advice was sought from the on-call consultant paediatrician in the nearest children’s hospital, 240 km away. He advised that the patient required an ECG to further investigate the arrhythmia. This posed a dilemma: the child gave a history consistent with COVID-19 at the time of an outbreak but was not critically unwell. No ECG machine was available in the coronavirus assessment centre, and arranging for the child to be transferred to the nearest emergency department for ECG would have resulted in a potentially contagious patient being treated in a designated ‘cold’ part of the hospital not set up for assessing infectious patients. To avoid this, a Kardia device was delivered to the patient’s mother by the coronavirus assessment centre driver, removing the necessity for direct contact with the patient. The Kardia device is a credit-card-sized recorder able to record a single-lead ECG for up to 5 minutes3. It has been shown to be reliable for detecting arrhythmias in children in a community setting4.
The rhythm strip generated was then sent directly from the phone of the patient’s mother to both the coronavirus assessment centre GP and the specialist in the children’s hospital, with no patient identifiable data attached to the traces. The rhythm was identified as sinus rhythm, with occasional premature atrial ectopics occurring within the T wave leading to dropped beats and non-compensatory R–R pauses, as shown in Figure 1. This benign explanation of the irregular pulse was then communicated to the patient’s mother. The time taken for rhythm analysis and discussion with the family was less than the travel time of the Kardia device back to the coronavirus assessment centre by the driver.
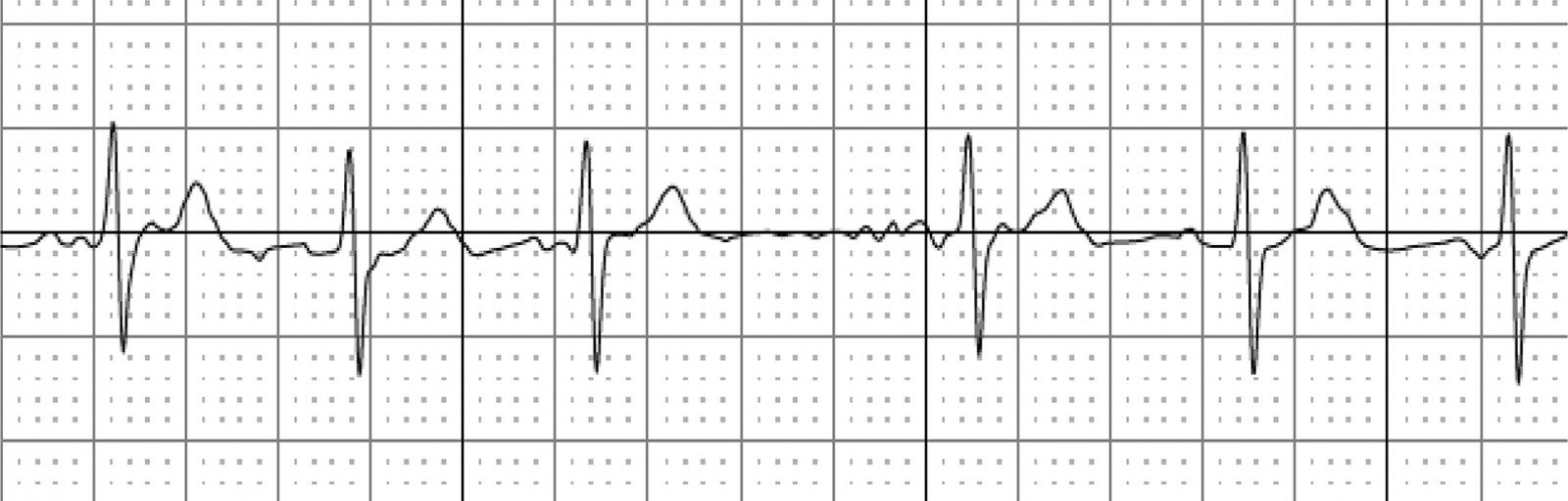 Figure 1: Extract from ECG, showing irregular QRS complexes.
Figure 1: Extract from ECG, showing irregular QRS complexes.
Differential diagnosis
This is a presentation with a wide range of differential diagnoses. The persisting fever with cough and nasal congestion supports a diagnosis of a viral upper respiratory tract infection. Transient arrhythmias have been shown to be associated with common viral respiratory infections5. Generally, upper respiratory infections require no treatment other than supportive care.
It is also possible this patient had a COVID-19 viral infection. Symptoms consistent with this include fever and dry cough, and many children have mild or no symptoms6. COVID-19 was known to be circulating in the local community at the time. There are reports of arrhythmias due to COVID-19 infection in both adult and paediatric populations7,8. Further investigation with ECG was felt necessary in order to pursue potential arrythmia, due to the identified irregular pulse.
Pneumonia is another possible explanation for the child’s presentation. The cough and elevated temperature would support this diagnosis. However the absence of tachycardia, increased work of breathing or raised respiratory rate suggest an alternative diagnosis9.
Treatment
No specific treatment was required for this patient. Advice about worsening symptoms, specifically mentioning other potential causes of fever such as urinary symptoms, rash, lymph node swelling and breathlessness, was given as well as advice regarding simple analgesia.
Outcome and follow-up
Two days after the consultation, the patient had returned to her usual good health. Subsequent severe acute respiratory syndrome coronavirus 2 polymerase chain reaction (PCR) testing of both the patient and her mother were negative.
Discussion
The COVID-19 outbreak has led to significant reorganisation of primary care. The primary care service in Scotland has centralised all COVID-19 assessment to phone triage bases, followed by assessment in specific coronavirus assessment centres where indicated.
The emphasis on remote consulting has reduced the risk of infection to staff members but introduces challenges regarding the best method for gaining more clinical information, should it be required. Drive-through oxygen saturation testing is one example of the novel types of patient assessment that are being introduced.
This case report describes the use of a mobile ECG recorder in a paediatric patient’s home to reduce potential exposure of staff to COVID-19. It highlights the benefits of instant electronic communication with geographically distant specialists to enable rapid diagnosis without the patient being required to attend a healthcare facility.
Remote consulting does not provide all the information clinicians are used to having available through examination and the nuances of non-verbal communication. The use of portable devices such as Kardia and pulse oximeters can provide more information to the clinician to aid decision-making at times when the clinician is encouraged to minimise contact with the patient.
Conclusion
There have been significant changes in the way patients are assessed in primary care due to the COVID-19 pandemic. The use of portable medical devices and electronic communication allows much work to be done without a patient leaving home.
The increase in use of telemedicine and physical distancing from patients can lead to diagnostic uncertainty due to the loss of both objective examination findings and the subtle cues gained from face-to-face consulting.
Despite pandemic conditions, patients still present with common illnesses. A subsequent negative COVID-19 PCR test result suggests the cause of this patient’s symptoms was most likely a more typical viral upper respiratory tract infection with benign arrhythmia.
References
You might also be interested in:
2013 - Retraction
