Introduction
Cardiovascular diseases (CVD) are the leading cause of death in Germany, with a total of 345 000 deaths in 20181. A considerable share of CVD-related disease burden is due to acute myocardial infarction (AMI). Age-standardised incidence of AMI was 354 per 100 000 among males and 163 per 100 000 among females in Germany in 20182. Although age-standardised incidence and mortality of AMI has decreased over the past two decades, the disease burden due to AMI remains an important public health problem2. At the same time, there is substantial heterogeneity of AMI mortality rates across the German federal states. The eastern federal states of Brandenburg and Saxony-Anhalt, both located in the former territory of the German Democratic Republic, had the highest AMI mortality in Germany in 2018. AMI mortality in Brandenburg is 50% above the national average and twice as high as in the former West German states of Hamburg and Bavaria3. Moreover, the prevalence of individual cardiovascular risk factors, AMI hospitalisation rates and AMI mortality of all five federal states of the former German Democratic Republic are significantly above the national average3-5.
An array of factors may account for the higher AMI incidence and mortality in the state of Brandenburg. Besides a high prevalence of established individual cardiovascular risk factors like diabetes mellitus, smoking, arterial hypertension, obesity and metabolic syndrome, structural factors such as socioeconomic deprivation and rurality may explain the high burden of CVD4,6. Socioeconomic deprivation has been defined as an index of occupational, educational and income-related regional characteristics7, and the concept has been developed to describe the material wealth of a region8. In Germany, socioeconomic deprivation is measured by the German Index of Socioeconomic Deprivation, which combines, inter alia, the proportions of people without school-leaving qualification, the proportion of unemployed people of working age, and the net household income7. The state of Brandenburg is located in the quintile of the highest socioeconomic deprivation in Germany, but deprivation itself is heterogeneous within Brandenburg7. Area-related socioeconomic deprivation might be a social determinant of CVD and AMI, as it is frequently associated with individual exposure to psychosocial stress, lifestyle risk factors, low adherence to preventative and acute treatment of CVD, and, finally, incidence and mortality of CVD and AMI9-15.
The rurality of a region is defined by the German Federal Institute for Research on Building, Urban Affairs and Spatial Development as a low population density combined with the lack of a regional centre16. Rurality may be accompanied with a deficient access to health care for patients with ischaemic heart disease6. In particular, deficient general primary care may lead to less optimal primary prevention of AMI and ultimately to an increase in AMI incidence17,18. The structural problems of the state of Brandenburg include a workforce deficit due to a lower number of outpatient cardiologists compared to the national average3. Moreover, longer distances to general practitioners (GPs), chest pain units and cardiac catheter labs (CCLs) are an additional factor that might influence prevention and health care of people at risk for ischaemic heart diseases3. However, studies on urban–rural differences of cardiovascular mortality showed heterogeneous results. While cardiovascular mortality in the USA was higher in rural compared to urban areas, a reverse association has been documented in Sweden9,19. It is difficult to draw a picture of the relative importance of socioeconomic deprivation and rurality, since few studies have examined mutually adjusted associations of both factors9. Finally, it has been suggested that the relationship of socioeconomic deprivation with mortality for ischaemic heart diseases might differ according to social and built environment9. The social environment is assumed to be shaped by specific cultural milieus, social norms and interaction patterns20. Furthermore, characteristics of the built environment such as population density, the availability of public transportation or healthcare infrastructure might moderate the association of socioeconomic deprivation with AMI9. In Germany, evidence of an association of socioeconomic deprivation with the occurrence of AMI is available from an urban setting in western Germany11. Evidence is missing from rural areas including areas in eastern Germany.
The aim of this study was to investigate the association of socioeconomic deprivation with AMI hospitalisation rates in a rural setting in eastern Germany. To draw a more detailed picture of the study’s setting, a map of social contextual characteristics together with information on transportation and healthcare-related infrastructure of the region was compiled.
Methods
Study design and population
A descriptive historical cohort study using pseudonymised routine data of the Hospital Brandenburg was conducted in the city of Brandenburg, Germany. All patients aged 18 years or more with a diagnosis of incident or recurrent AMI who were treated in the Hospital Brandenburg between 1 May 2019 and 30 May 2020 were included in the study. A study nurse identified all patients discharged with the International Classification of Diseases (ICD)-10 code I21 using the hospital´s electronic data system. To ascertain a high quality of the case definition, a study nurse reviewed the clinical records of all identified cases for any disagreement with the ‘Fourth universal definition of myocardial infarction’ published by the European Society of Cardiology (ESC). The ESC defines AMI as the detection of a rise and/or fall of cardiac troponin with at least one value above the 99th percentile upper reference limit and with at least one of the following: symptoms of acute myocardial ischaemia, new ischaemic ECG changes, development of pathological Q waves in the ECG, imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischaemic aetiology, identification of an intracoronary thrombus by angiography or autopsy21. In a second step, a check for any non-cardiac cause for elevated cardiac troponin was performed among patients with no ST elevation in the ECG, using the routinely documented diagnostic workup until 48 hours after the initial cardiac troponin test. A physician checked all decisions by the study nurse. This procedure revealed two cases that did not display an unequivocal cardiac cause of elevated troponin.
To calculate hospitalisation rates, the catchment area of the Hospital Brandenburg for the treatment of acute AMI was defined. The catchment area included all postal code areas that were highly likely to refer almost all patients with AMI to the Hospital Brandenburg. To identify postal code areas that were located entirely within the catchment area, all locations of neighbouring CCL were mapped. Postal code areas were included if road travel time from the most distant places of each postal code area to the Hospital Brandenburg was shorter than road travel time to any other CCL. Consultants of the department of cardiology reviewed the selected areas. Based on this process, 10 postal code areas were included. All included postal code areas were numbered and mapped (Fig1). Census data were used to derive population time for each postal code area. These data were provided by the statistical offices of the states of Berlin and Brandenburg22. The population counts of each postal code area from 31 December 2018 were used and stratified by sex and 10-year age groups. The population counts were divided by 12 to yield person time per month.
Data collection and assessment of variables
Data on age, sex, month of diagnosis, place of residence, body mass index, as well as data on prevalent arterial hypertension, hyperlipoproteinaemia, coronary heart disease, diabetes mellitus and stroke for each patient with AMI were collected from medical records. The data were entered into the EDC-system SecuTrial®, which automatically checked for errors, completeness, validity and inconsistencies when information was entered in the electronic case report form. Age was categorised into 10-year age groups. The driving distance from AMI patients’ places of residence to their GP was calculated if information on a GP was available. In addition, the distance to the CCL at the Hospital Brandenburg and the time from the beginning of symptoms to the admission to hospital were calculated from information contained in the medical records for all AMI patients.
Recent evidence showed a considerable decrease of admissions with AMI after the onset of the COVID-19 pandemic in March and April 2020 in Germany23. To allow adjustment of results by period, the time period 1 May 2019 to 28 February 2020 was categorised as the period before the COVID-19 outbreak in Germany, and the time of 1 March 2020 to 30 May 2020 was categorised as the period during the outbreak.
Deciles of the German Index of Socioeconomic Deprivation for 2012 were used to define the exposure variable7. The four postal code areas of the city of Brandenburg were within the decile of the highest socioeconomic deprivation (10th decile). Among the six neighbouring postal code areas, five were equal or below the fifth decile and one was in the ninth decile. Hence, the city of Brandenburg was defined as a region with high socioeconomic deprivation, and all adjacent areas were combined and classified as areas with medium deprivation.
A map was made to describe further social contextual characteristics, together with transportation and healthcare-related infrastructure of the study area using the software package QGIS Geographic Information System v3.4.1 (QGIS Development Team; http://www.qgis.osgeo.org). The study authors used the publicly available data of the platform of the German Census 2011 and the platform Indicators and Maps for Development of Spaces and Cities (INKAR)24,25. In addition, the database of the Association of Statutory Health Insurance Physicians of the state of Brandenburg (record date 1 May 2018) was searched for all GPs, GPs who specialised in internal medicine and cardiologists within the study region, and their locations were mapped.
Statistical methods
Numbers of observations and proportions according to sociodemographic and clinical characteristics of all cases with myocardial infarction were calculated to describe the sample. Medians and interquartile ranges (IQRs) of distances and time from the beginning of symptoms to admission at hospital were calculated for patients from the area of high deprivation (city of Brandenburg) and patients from the areas of medium deprivation (neighbouring municipalities). Medians were compared between both areas using Wilcoxon rank-sum tests. Crude hospitalisation rates of AMI with 95% confidence intervals (95%CI) were calculated for females and males according to categories of area deprivation. Poisson regression was used to calculate age-, sex- and period-adjusted ratios of hospitalisation rates in areas with medium deprivation compared areas with high deprivation. Rates were modelled using monthly counts of AMI as the numerator and person-time per month as the denominator. Sex-specific rate ratios were derived using an interaction term of area deprivation with sex in the Poisson regression model. Robust standard errors were used to calculate p-values and 95%CI of rate ratios26. Moreover, the authors performed a sensitivity analysis of the results from Poisson regression to assess the possible impact of an overlap of catchment areas of neighbouring hospitals with the Hospital Brandenburg for the treatment of AMI. Therefore, postal code areas 6, 7 and 8 of the study area (Fig1) that were close to neighbouring CCLs were excluded and all regression analyses repeated. R software v4.0.2 (R Core Team; http://www.r-project.org) was used to conduct statistical analyses.
Ethics approval
The ethics committee of Brandenburg Medical School approved this study (E-01-20200923).
Results
A total of 265 patients with AMI between May 2019 and May 2020 and the main place of residence in the study area are included. Of these, 82 patients (30.9%) were female and the majority were aged over 60 years (Table 1). Eighty patients (30.2%) had their main place of residence in areas with medium deprivation (neighbouring municipalities) and 56 (21.1%) patients were admitted between March 2020 and May 2020 (during the COVID-19 outbreak). There were no missing observations related to sex, age group, area deprivation, time of beginning of symptoms and time of hospital admission. Clinical characteristics of all cases are displayed in Table 1. Of all patients, 201 (75.8%) had hypertension, 141 (53.2%) had hypolipoproteinaemia, 95 (35.8%) had previously diagnosed coronary heart disease, 96 (36.2%) had diabetes mellitus and 16 (6.0%) had experienced a stroke prior to admission. There were 6 (2.3%) missing observations for hypolipoproteinaemia and 14 (5.3%) missing observations for body mass index.
The study area included a total population of 116 126 inhabitants in 2018. Figure 1 displays a map of the defined catchment area of the Hospital Brandenburg. The red line shows the area of the highly deprived city of Brandenburg. The characteristics of the city of Brandenburg and its adjacent areas are displayed in Table 2. The population density of the city of Brandenburg was five times higher than in neighbouring municipalities. According to the German Federal Office for Building and Regional Planning the city of Brandenburg is classified as a medium-sized town. Among the neighbouring municipalities, three are classified as small towns and 11 are classified as rural municipalities16. The proportion of people aged over 70 years, people of foreign nationality and people living in a single household were higher in the city of Brandenburg. The number of public bus and train stations per 10 000 inhabitants was higher in neighbouring municipalities, while the number of hospital beds per 10 000 inhabitants was higher in the city of Brandenburg. The number of GPs per 10 000 inhabitants did not differ between the two areas. Among all patients with AMI, the median distance to the GP (p=0.01) and the median distance to the Hospital Brandenburg (p<0.001) were lower in the city of Brandenburg compared to neighbouring municipalities (Table 3). The median time from beginning of symptoms to admission at hospital did not differ between the two areas.
Crude hospitalisation rates of AMI were 139.1 per 100 000 population (95%CI 104.8–181.0) among women living in areas of high deprivation and 113.1 per 100 000 (95%CI 74.5–164.5) among women living in areas of medium deprivation. Among men, these rates were 336.9 per 100 000 (95%CI 281.5–400.1) in areas of high deprivation and 222.7 per 100 000 (95%CI 166.8–291.4) in areas of medium deprivation. The sex- and age-adjusted hospitalisation rate was 29% lower (p=0.01) in areas with medium deprivation compared to the highly deprived city of Brandenburg (Table 4). Interaction analysis revealed that the age-adjusted hospitalisation rate in areas with medium deprivation was 86% of the rate in areas with high deprivation among women (p=0.51), and for men the medium deprivation rate was 65% of that in areas with high deprivation (p=0.003). There was no evidence for effect measure modification by sex (p for interaction=0.33). When postal code areas close to a neighbouring CCL (areas 6, 7 and 8) were excluded, the results were comparable. The sensitivity analysis was based on a total population of 96 404 and 211 cases of AMI. The sex- and age-adjusted rate ratio comparing areas with medium deprivation to areas with high deprivation was 0.56 (95%CI 0.38–0.83, p=0.004). Among females and males, the age-adjusted rate ratios were 0.37 (95%CI 0.16–0.86, p=0.02) and 0.64 (95%CI 0.41–1.00, p=0.05), respectively. There was no evidence for effect measure modification by sex (p for interaction=0.27).
Table 1: Description of sociodemographic and clinical characteristics of all cases with acute myocardial infarction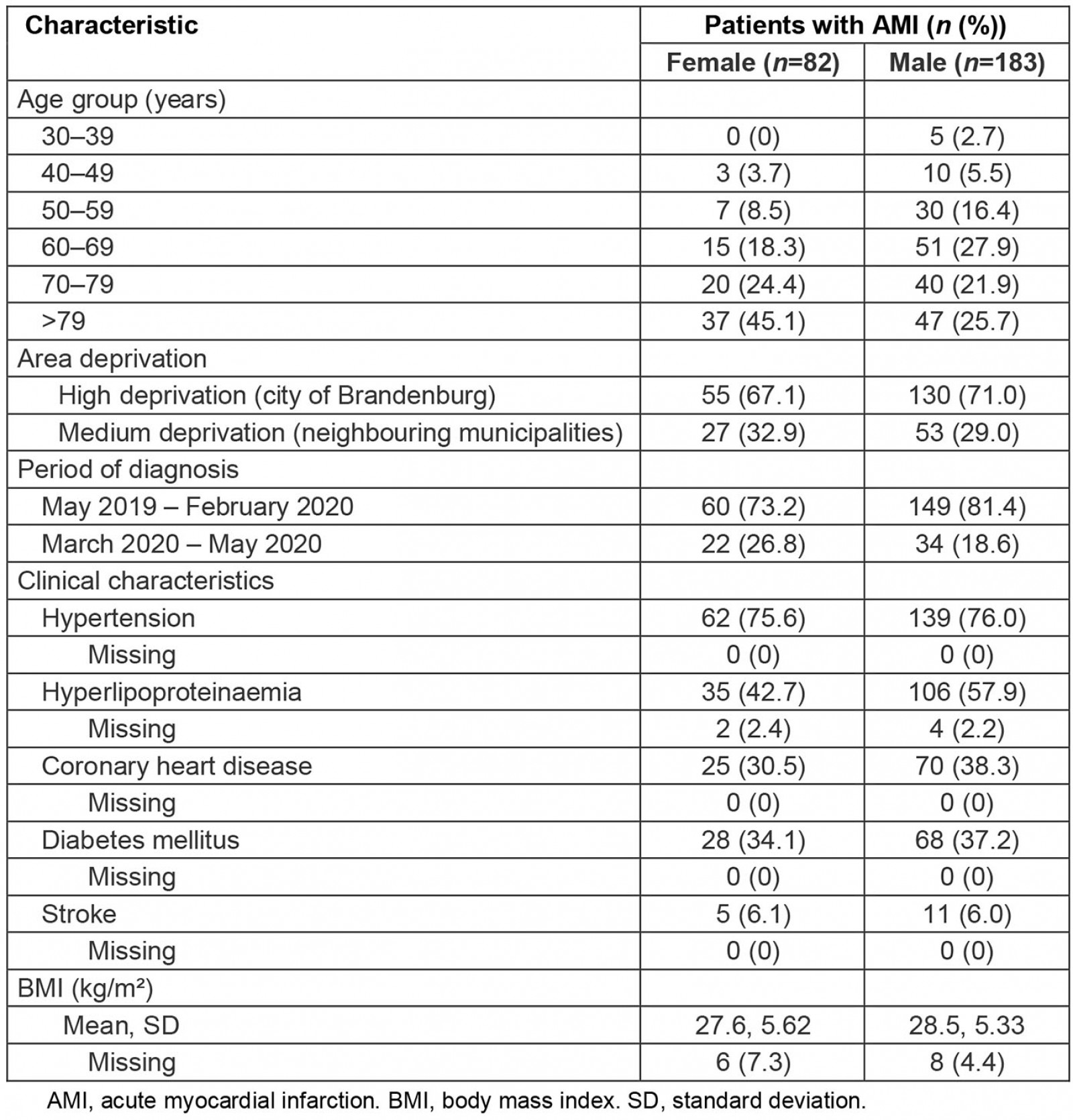
Table 2: Social, transport-related and healthcare-related characteristics in the city of Brandenburg and in neighbouring municipalities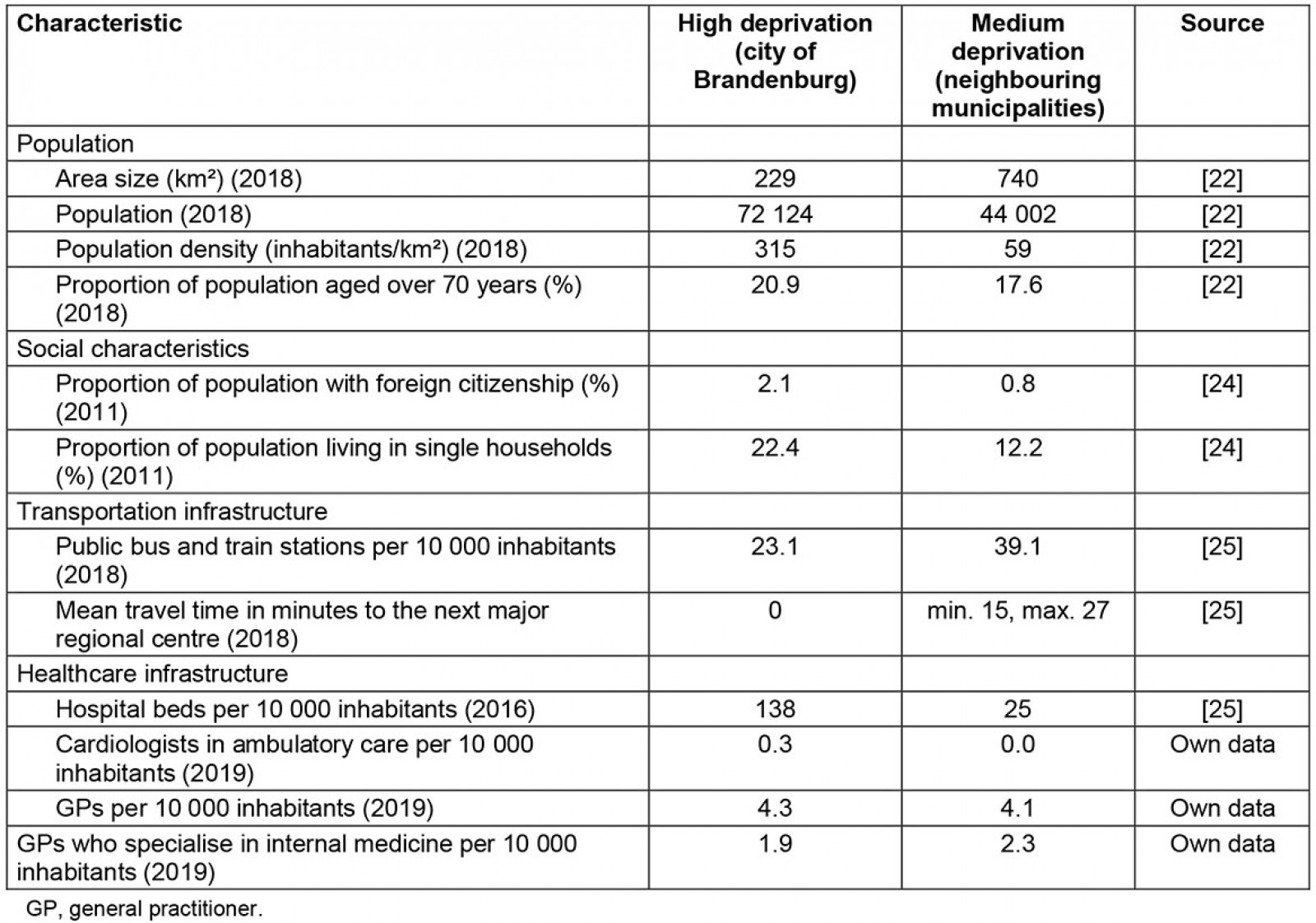
Table 3: Distance to general practitioner, distance to the Hospital Brandenburg and time from beginning of symptoms to admission at hospital among cases with acute myocardial infarction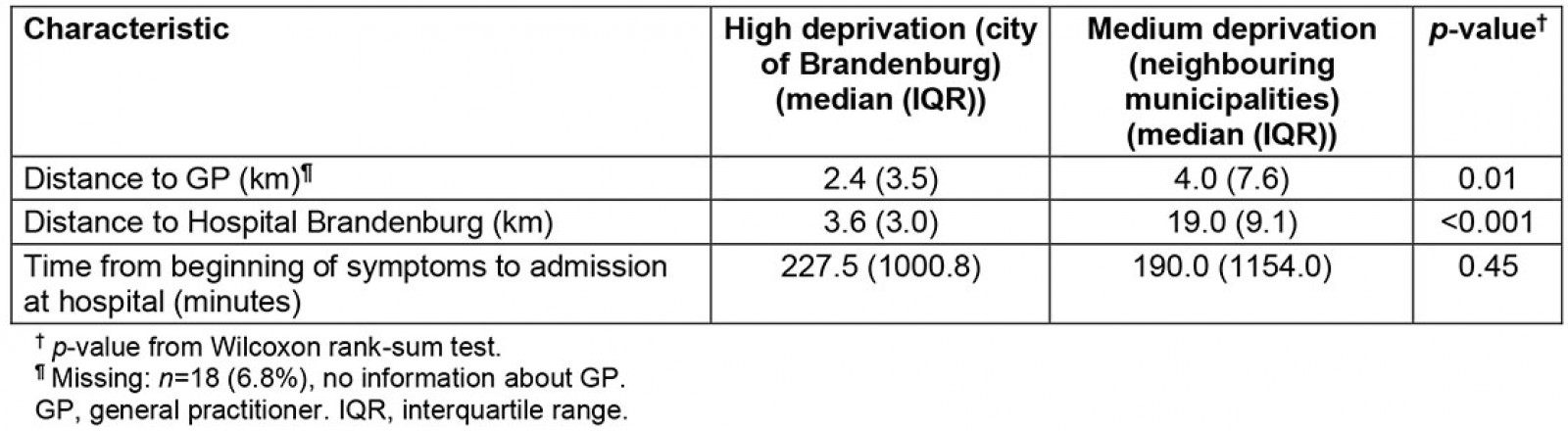
Table 4: Adjusted rate ratios comparing hospitalisation with acute myocardial infarction in medium deprived areas to the highly deprived city of Brandenburg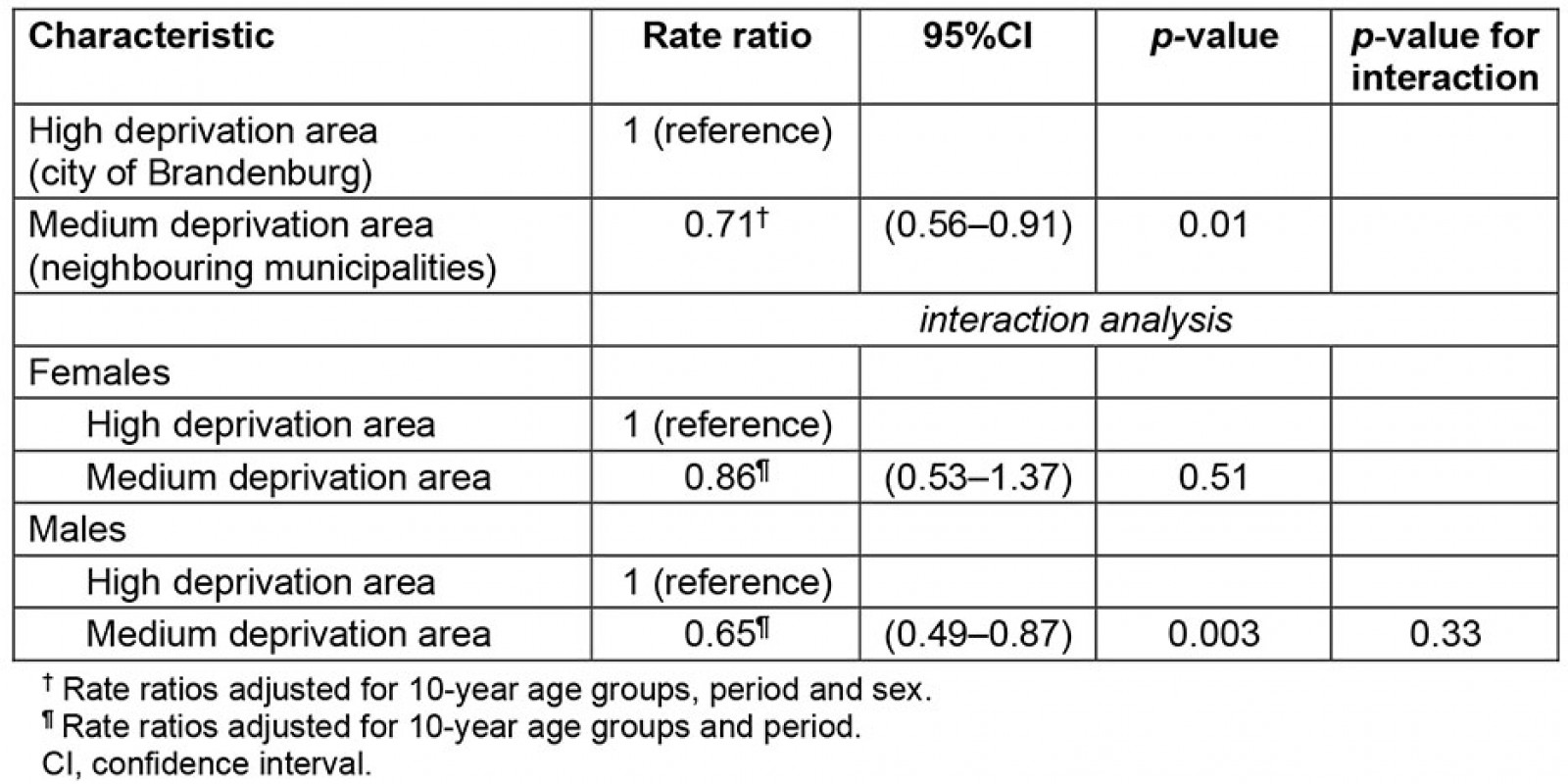
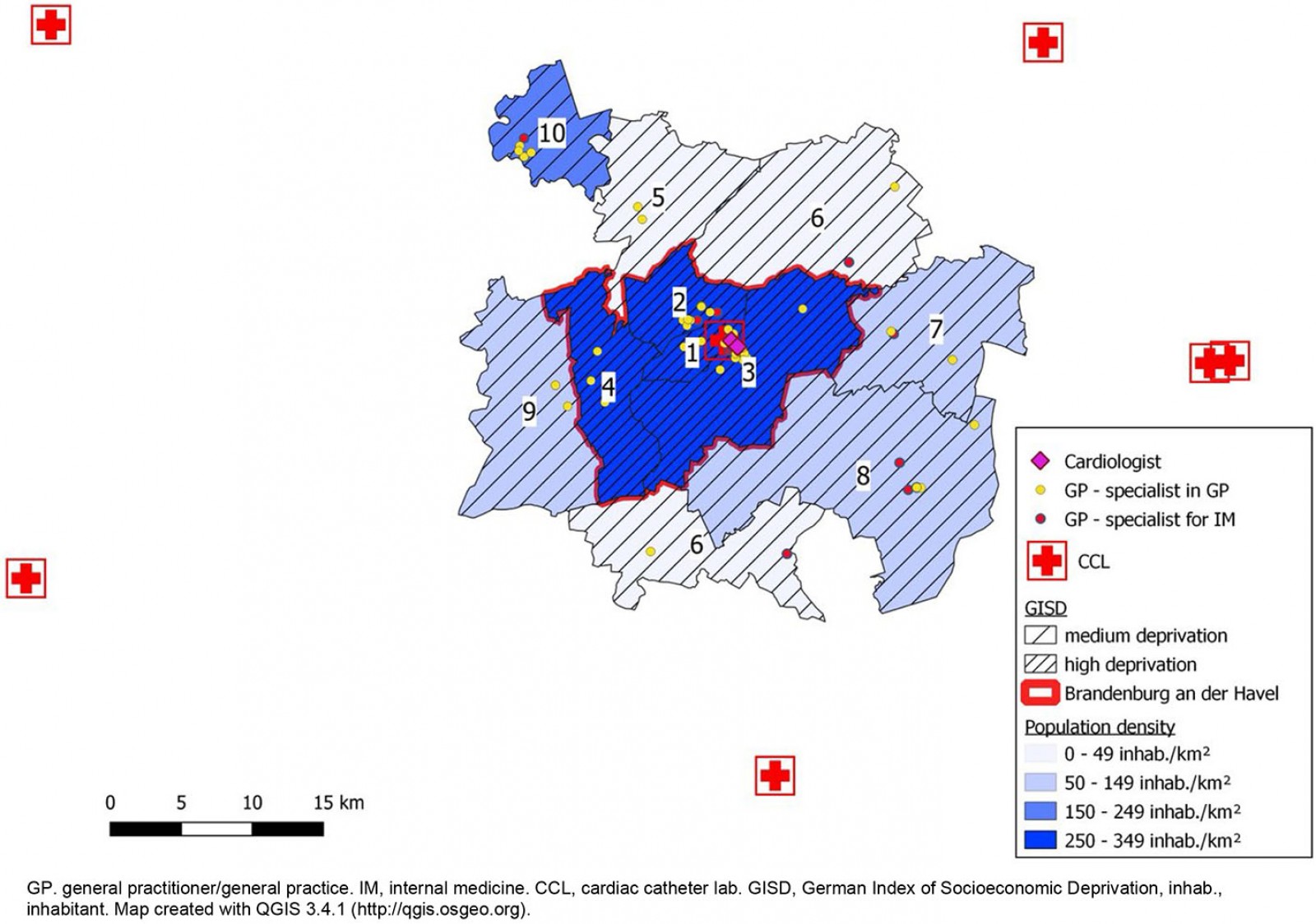 Figure 1: Map of the catchment area of the Hospital Brandenburg, Germany, for the treatment of acute myocardial infarction.
Figure 1: Map of the catchment area of the Hospital Brandenburg, Germany, for the treatment of acute myocardial infarction.
Discussion
Among 265 patients hospitalised with AMI between May 2019 and May 2020, 80 had their main residence in the municipalities surrounding the city of Brandenburg. The hospitalisation rate was higher in the highly deprived city of Brandenburg compared to adjacent areas with medium deprivation after adjustment for age, sex and period. Besides a high socioeconomic deprivation, the city of Brandenburg was characterised by higher proportions of inhabitants over 70 years, living in single households and with foreign citizenship. The number of GPs per 10 000 inhabitants and the time from beginning of symptoms to admission at hospital of cases with AMI did not differ between both areas.
The review of all cases with AMI depicts a strength of this study. The authors decided to review all cases using routinely documented data for disagreement with the ESC definition, since this definition of AMI is mainly based on the increased levels of cardiac troponin21. In case of non-ST elevation myocardial infarction at hospital admission, some cases may reveal a cause for elevated troponin levels other than myocardial ischaemia during hospital treatment. Accordingly, these patients had to be identified and excluded. This problem was solved by monitoring the routinely documented diagnostic workup of all cases that were identified. In two cases, a cardiac cause could not be confirmed unequivocally. This procedure indicated an acceptable quality of outcome data. However, since the review was based on routine data only, there remains some uncertainty regarding the accuracy of the case definition of AMI.
This study’s comparison of hospitalisation rates between areas with high and medium deprivation is valid, if ascertainment of hospitalised patients with AMI in the entire study area is complete. Therefore, the catchment area was carefully defined using postal code areas that were highly likely to refer all cases with AMI to the Hospital Brandenburg. The most remote part of the postal code area in the north-east of the study region overlaps with the catchment area of the neighbouring CCL. All other postal code areas do not overlap with catchment areas of other CCL. However, an exclusion of the postal code areas close to the neighbouring CCL neither changed the magnitude of rate ratios nor their levels of significance. Therefore, the authors are confident that the choice of the catchment area did not introduce selection bias. Population data from 31 December 2018 was used because population data for 2019 and 2020 were not yet available from the statistical office Berlin-Brandenburg. The annual change of population numbers in the catchment area did not exceed +0.5% in the past 4 years and the trend did not differ between the city and neighbouring municipalities22. Hence, it is assumed that the rate ratios comparing both areas are unlikely to be biased due to different population trends in both areas during observation. Finally, hospitalisation rates, rather than incidence of AMI, were measured. Hence, results were influenced by both risk factors for the development of AMI and factors that influence prognosis after first occurrence of the disease.
The results of this study are in line with national and international studies that found an association of high socioeconomic deprivation with incidence of AMI9-11,13. However, the relative importance of socioeconomic deprivation, rurality and further contextual characteristics is still unresolved. For example, a cohort study on cause-specific cardiovascular mortality showed a stronger effect of population density compared to average regional income9. Research on contextual effects is complicated by the fact that regional characteristics are often highly collinear27. Similarly, the urban area in this study was also the most socioeconomically deprived region, and independent associations of deprivation and rurality could not be assessed. Moreover, the exact causal pathway between socioeconomic deprivation and AMI is yet to be determined. Several factors, such as social cohesion, cultural norms, the availability of material resources, prevalence of lifestyle-related risk factors and barriers to public amenities have been discussed as mediating factors of the relationship15. Finally, the results suggest that the time from the beginning of symptoms until admission to hospital did not differ between AMI patients from the city and patients from neighbouring areas, indicating no delayed emergency care in rural areas. This finding is surprising because the distance to CCL is significantly longer in neighbouring municipalities. However, this result should be investigated in more detail in future research, complemented with further and more valid measures such as contact-to-balloon time.
Considering the picture of regional characteristics in the study area, the authors hypothesise that the high hospitalisation rate of AMI in the city of Brandenburg might be explained with the higher socioeconomic deprivation in comparison to neighbouring areas. The rural character and the lower availability of specialist care in neighbouring areas were not associated with higher hospitalisation rates of AMI compared to the city. In the state of Brandenburg, the rural character of most districts is often discussed as an important target for preventive measures and healthcare delivery, because average distance to specialist care is longer than in other federal states3. In addition, primary health care in rural areas might deteriorate in the future, since a significant proportion of physicians in the ambulatory sector will retire in the next few years28,29. The results suggest that both socioeconomic deprivation and rurality should be considered when planning resource allocation for cardiovascular health in Brandenburg. This notion can be supported by a recent study on regional health inequalities in Germany, which found that life expectancy is lower in areas with high proportions of unemployment and people on social benefit compared to less deprived areas. As there were little differences of life expectancy on account of rurality, the authors of the study proposed to focus on socioeconomically deprived areas rather than on rural areas alone to improve health30. Studies from Germany on survival after cancer diagnosis are supporting this argument. While little difference in survival has been documented in rural compared to urban regions, survival is lower in socially deprived compared to more affluent areas31,32.
Conclusion
This study found that hospitalisation rates are higher in the socioeconomically deprived city of Brandenburg compared to the less deprived surrounding areas. Since this study was a descriptive study of a single area in eastern Germany, the study findings need to be confirmed by population-wide prospective studies before conclusions can be generalised to larger populations. Future studies should aim to consider confounders related to the social and built environment when assessing the association of socioeconomic deprivation with AMI occurrence.
Acknowledgements
The authors would like to thank all participating patients and the team of study nurses Jacqueline Adamczewski, Sarina Walter, Stefanie Baum, Saskia Steinbeiß, Uta Hiller and Linda Weiland. In memoriam of Sarina Walter.
References
You might also be interested in:
2011 - Colorectal cancer screening among rural Appalachian residents with multiple morbidities

