Introduction
Motor vehicle collisions (MVCs) are a major contributor to premature mortality, presenting a significant public health challenge1. Road traffic fatalities reached 1.35 million in 2016 and are the leading cause of death for children and young adults globally2. Of the 35 OECD nations, Australia’s and Canada’s fatality rates are just above the median3. Though trends over time in both countries indicate road traffic deaths are declining, fatality rates remain significant at 4.68 per 100 000 (2019) in Australia and 4.69 per 100 000 (2019) in Canada. MVC fatalities result in a large economic burden which is estimated at 1.3% of GDP in Australia, and 2.2% in Canada4,5. From 2010 to 2019, the average annual change in road deaths was –2.3% in Australia and –2.9% in Canada3. The number of road fatalities has significantly decreased following lockdown restrictions in response to the COVID-19 pandemic; however, preliminary data suggest fatality rates have not decreased in proportion to the decrease in traffic6. Globally, although absolute numbers of MVCs have reduced during COVID-19, there has been a relative increase in the severity of injury and death7. The WHO has predicted that, without higher investment and evidence-based interventions, Sustainable Development Goal target 3.6 to ‘halve road traffic deaths by 2030’ will not be achieved2.
MVC fatalities in rural areas have been identified as high in comparison to their urban counterparts8. Remote and rural areas present unique road safety challenges. Vehicles typically travel on rural roads at faster speeds, for longer distances, in lower quality road conditions9. The risk of fatality following a rural MVC is increased due to overstretched and low-resource health services, distance to high-level trauma services and difficult access to the scene of the incident for emergency vehicles10.
Prevention methods for rural road fatalities must consider the complexities of rural road fatality determinants and the challenges linked to rurality, requiring a multifaceted approach. Proposed strategies include improved road design, effective education campaigns, programs to reduce unsafe driving behaviours, and reduction of rural speed limits. However, understanding what this looks like from a rural perspective will be critical for effectiveness5. Rural road prevention strategies to date have received insufficient attention10.
There is limited research from high-income countries comparing geographical variations in rural traffic fatalities. Comparisons of Australia and Canada, which have similar rural health challenges, population density, universal healthcare systems and political structures, allow for the identification of cross-nation risk factors and effective strategies11. However, it is expected that some notable differences will exist due to factors such as weather-related road conditions and unique geographical challenges.
The aim of this review is to compare and contrast the epidemiology, risk factors and prevention strategies of rural road fatalities for Australia and Canada.
Methods
A scoping literature review was undertaken systematically according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) protocols 2009 statement12. Original peer-reviewed studies published in English from 2000 to 2021 were identified using the databases EMCARE, Medline, CINAHL, Scopus and Informit. Slight search term variations were used depending on the database to maximise results (Supplementary file 1). Keywords included ‘Australia’ or ‘Canada’; ‘traffic incident’; ‘rural’ or ‘remote’; ‘death’ or ‘fatality’ (see Supplementary file 1 for the detailed search design).
Papers included in the review met the following criteria: (1) fatalities were unintentional, (2) primary Australian and/or Canadian data were utilised (3) reference was made to risk factors, prevention strategies and/or fatality rates for rural MVCs. Studies regarding offroad vehicle fatalities, on-farm and intentional fatalities (suicide) were excluded. Review articles, letters to editors, conference proceedings, dissertations and technical reports were also excluded.
Initial search results were exported into Endnote vX8 software. Duplicate entries were removed, titles and abstracts were screened and full-text reviews were undertaken by the principal reviewer, then checked by a second author. Articles were selected based on their compatibility with the study aims and inclusion criteria. Reference lists were scanned to identify additional relevant studies, and this yielded no additional results. The quality of each article was assessed using a checklist adapted from McMaster University’s Quality Review Form by author HM and double-checked by author RF13. Twelve items that were appropriate for retrospective analyses were included in the checklist. The items included study purpose, background literature, ethics, design, sample, presentation of results, potential bias, and conclusions and implications13.
Data were extracted from each article into a spreadsheet, including author names, year of interest, region of study, number of participants, study design and data sources. Relevant epidemiological measures were obtained from articles where they were presented. Where these values were not available, risk ratios plus 95% confidence intervals (CIs) were manually calculated if possible. A meta-analysis based on relative risk was undertaken using Comprehensive Meta Analysis v3.3.070 (https://www.meta-analysis.com).
Risk factors were defined as any attribute, characteristic or exposure that increased the likelihood of a fatal road crash14. Factors that were identified as risk of a crash event or injury but not fatality were excluded. Significant rural MVC fatality risk factors identified in the literature were extracted, categorised, and their frequencies were recorded.
Prevention strategies were defined as any proposed intervention or activity implemented to reduce rural MVC fatalities. Prevention strategies in the review were evaluated on their level of evidence and grouped to identify patterns and consistencies.
Results
The initial literature search included studies from January 2000 to December 2019 and yielded 326 articles. The search was updated to include literature from 2020 to June 2021, which yielded an additional 38 articles. After removing duplicate entries, 266 titles and abstracts were organised according to the inclusion criteria, and 50 articles were included for full-text appraisal. A total of 43 studies were selected for the final review (Fig1). Of these, 13 were Canadian-based studies, 29 were Australian-based studies, and one was both Australian and Canadian. Fourteen studies included epidemiological information, 25 included fatality risk factors and 37 identified prevention strategies.
Of the included studies, 42 were quantitative (97.7%), and one was qualitative (2.3%) (Supplementary file 2). Regarding study design, 25 were retrospective, population-based studies (58.1%), 11 were retrospective cohort studies (25.6%), two were cross-sectional (4.7%), one was a prospective cohort study (2.3%), one was a qualitative evaluation study (2.3%), one was a descriptive case analysis (2.3%), one was a before-and-after evaluation (2.3%), and one used a combination of retrospective cohort and cross-sectional methods (2.3%) (Supplementary file 2).
The overall quality of the papers was high, with 93% scoring at least 10/12 items on the checklist (Supplementary table 2). Most studies included a clearly stated objective, relevant background material, appropriate study design, justified sample size, reliable and valid outcomes, appropriately analysed results stated in terms of statistical significance, and appropriate conclusions. However, the following issues were identified: lack of sample description (n=8), missing ethics statement (n=23) and no reported limitations (n=7).
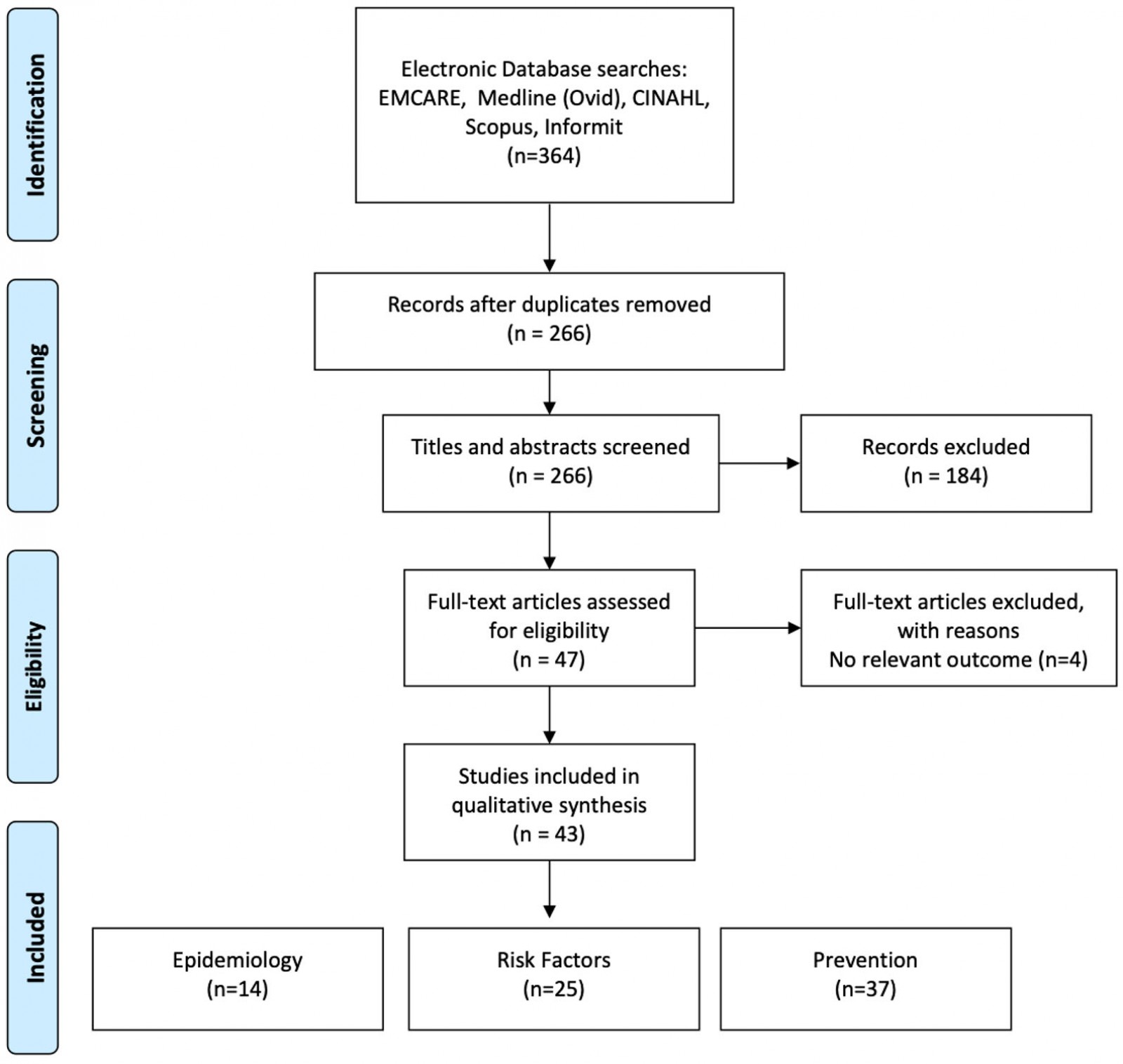 Figure 1: PRISMA flow diagram for scoping literature review12
Figure 1: PRISMA flow diagram for scoping literature review12
Epidemiology
Fourteen epidemiological papers were identified, of which eight were based on Australian data, five on Canadian data, and one utilised a combination of Australian and Canadian data (Table 1). Two studies reported based on national data, with the remaining 12 reporting on provincial, state or territorial data. Twelve reported relative risk data, one hazard ratios and one standardised mortality ratios. All studies indicated that those living in rural and remote areas were at higher risk of MVC fatalities in comparison to their metropolitan counterparts. In both countries, rural populations were more likely to die in an MVC, with the risk ratio for all ages ranging from 2.06 to 6.98 in Australia and from 2.55 to 5.40 in Canada. It was also determined that, in the event of a collision, the rural population was more likely to have a fatal outcome15. The highest relative risk (18.50; 95%CI: 4.14–82.74) was determined for rural versus urban children in Victoria, Australia aged 10–14 years16. Where standardised mortality ratios for biological sex were calculated, it was found that all rural categories for men and women were at increased risk in comparison to urban areas for both Canada and Australia11.
The meta-analysis revealed that people living in rural locations are 3.23 (95%CI: 3.01–3.48) times more likely to die in MVCs than their urban counterparts (Table 2, Fig2).
Table 1: Risk of fatality for rural versus urban crashes10,11,15-26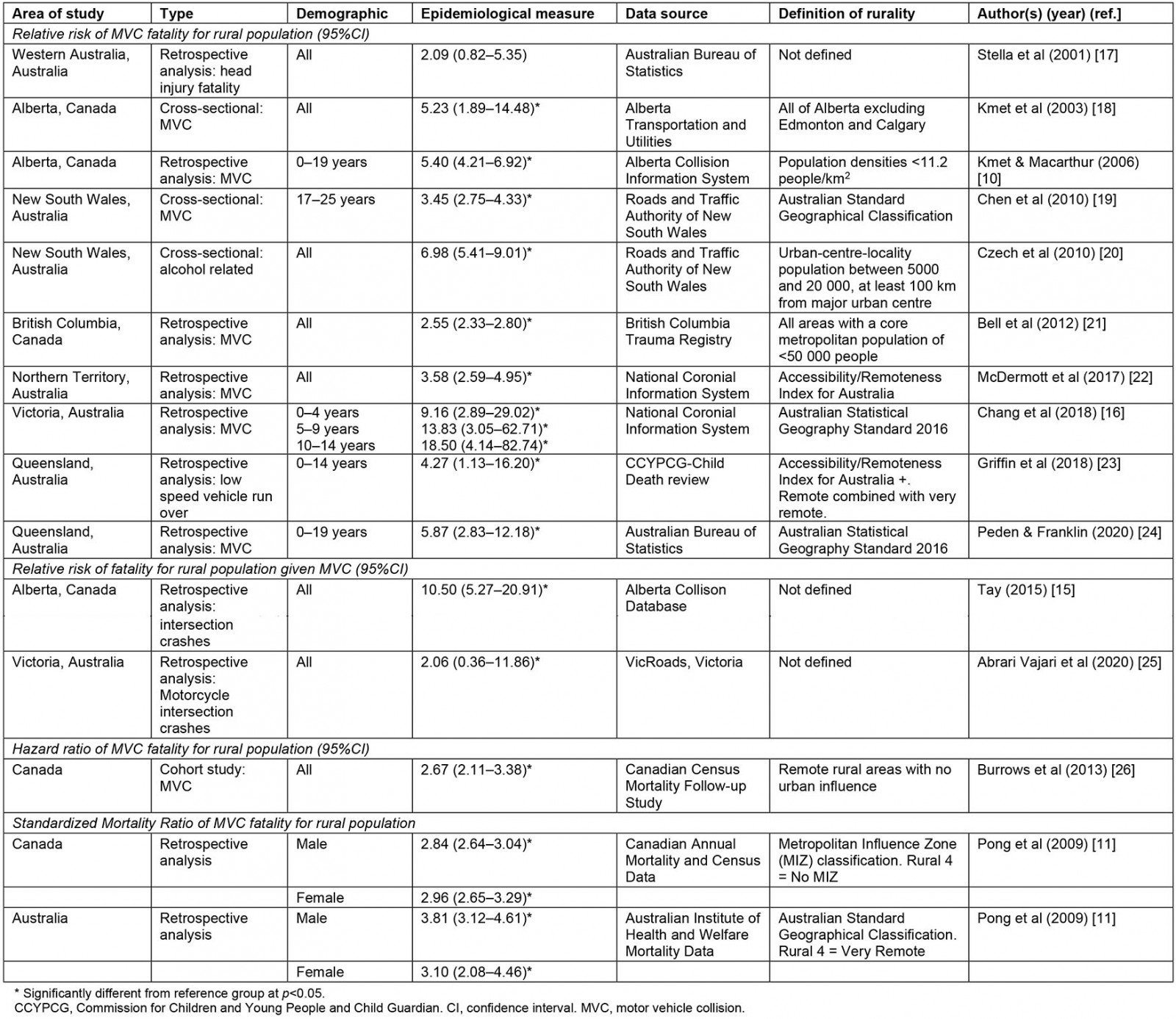
Table 2: Meta-analysis of relative risk of rural road fatalities in Australia and Canada10,15-19,21-23,25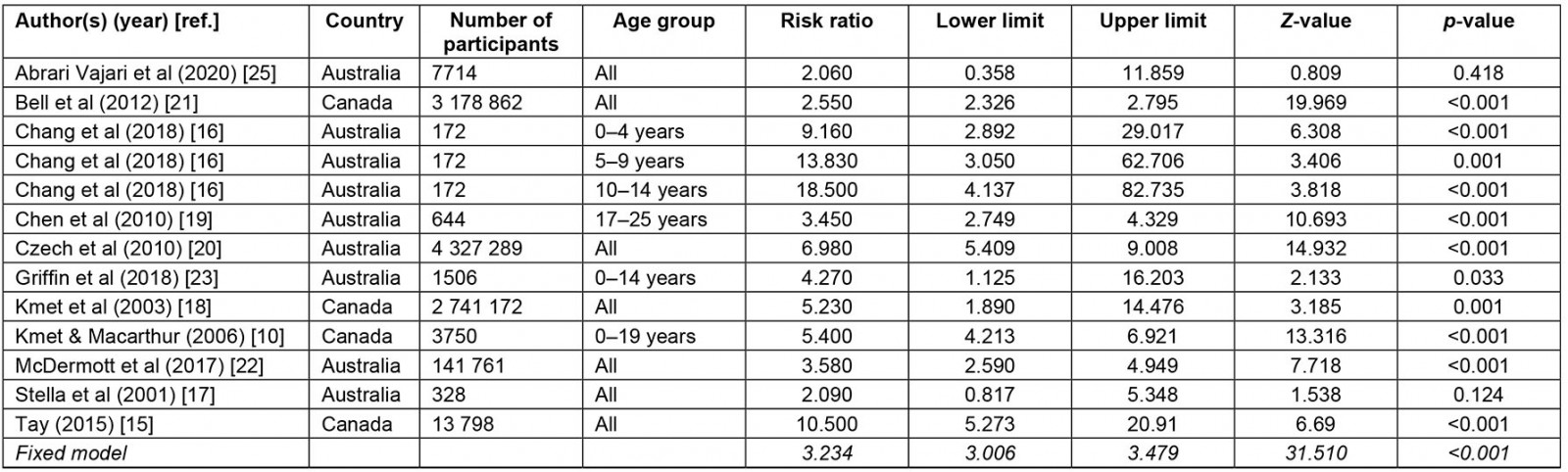
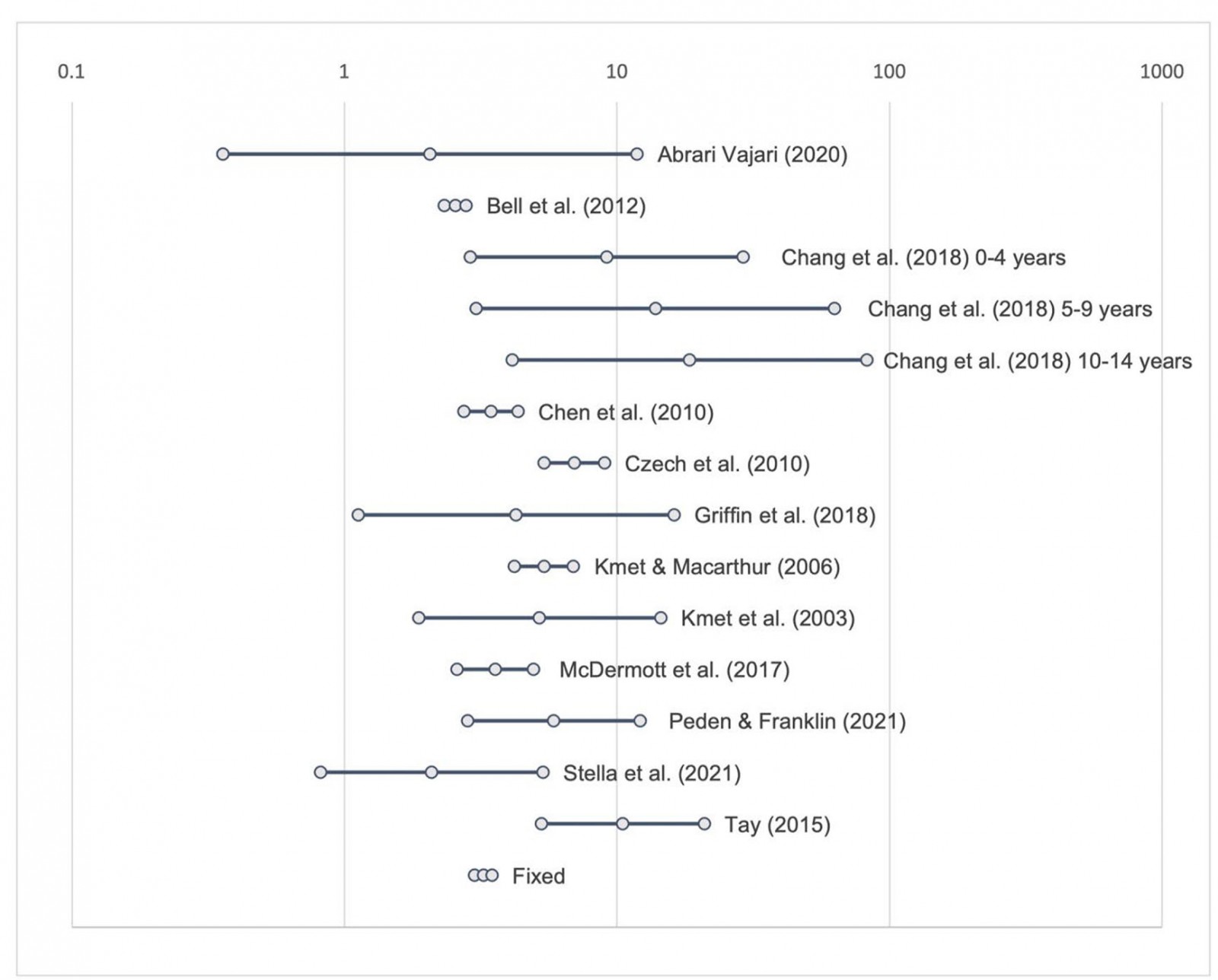 Figure 2: Risk ratio for meta-analysis of relative risk of rural road fatalities in Australia and Canada
Figure 2: Risk ratio for meta-analysis of relative risk of rural road fatalities in Australia and Canada
Risk factors
From the 25 studies that investigated risk factors for rural road fatalities, 15 factors were identified. These included drugs and alcohol, speed, age, driver error, biological sex, road design/condition, stationary objects, time of day, weekend, animal, risky illegal driving, low socioeconomic status (SES), motorcycle, wet season and travelling to health appointments (Table 3). The most acknowledged risk factor was driving under the influence of drugs or alcohol. There were no significant risk factors identified exclusively in rural Canada studies, but those identified in rural Australia studies were driver error, stationary objects, animals, risky illegal driving (driving without a licence, in a stolen vehicle or involved in a police chase) and travelling to obtain health care.
Studies that indicated biological sex as a non-modifiable risk factor determined males were more likely to be involved in a rural MVC fatality, apart from Ostry, who identified females aged 0–4 years as being at the highest risk27, and Peden and Franklin, who identified a higher proportion of road transport deaths for females aged 10–14 years in very remote areas24. Where age was considered a non-modifiable risk factor, the age groups identified were 0–2 years, 0–4 years, 15–19, 15–25 and 75 years or older.
Table 3: Risk factors for rural road fatality24,27-41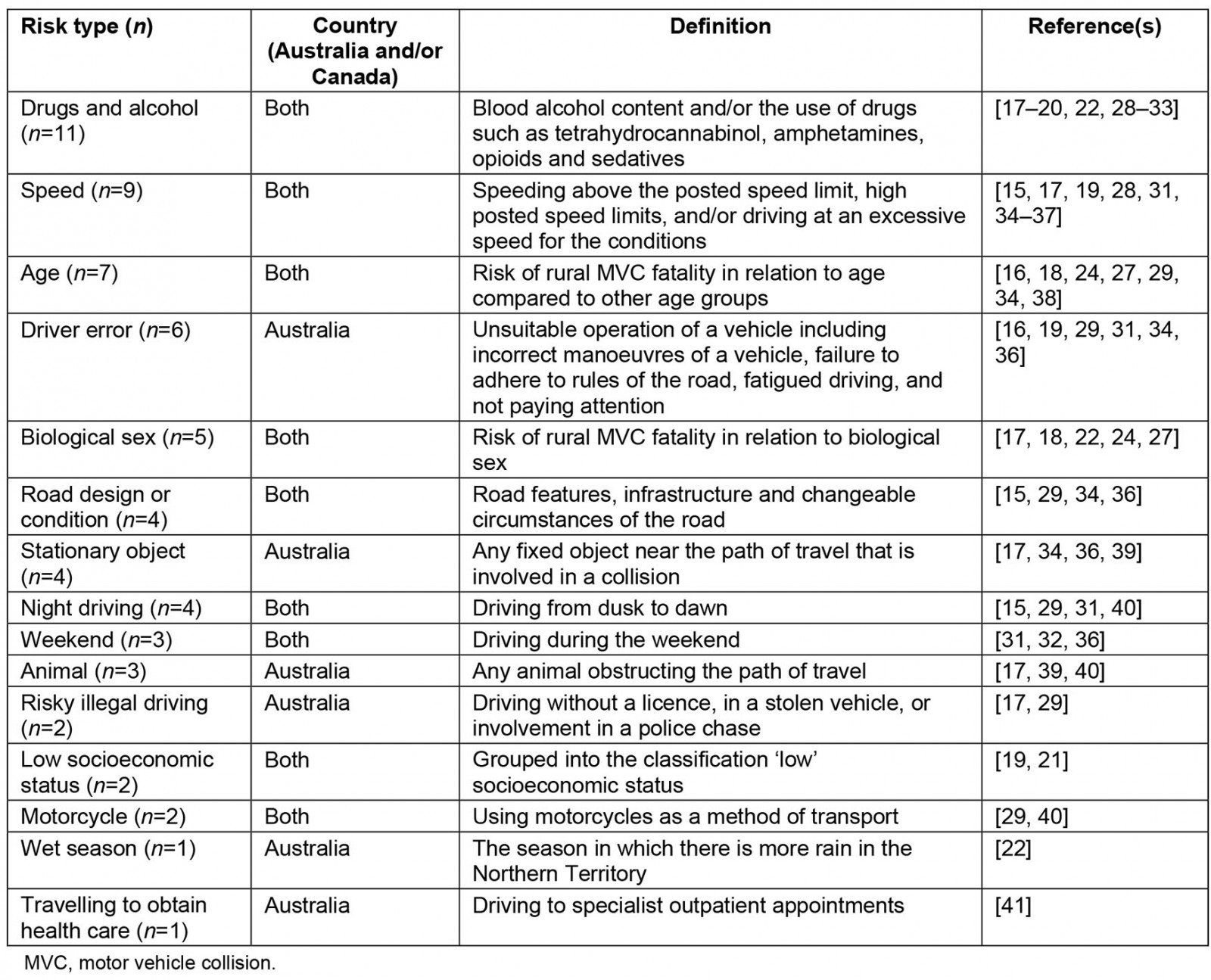
Prevention strategies
There were 37 articles that suggested prevention strategies and three studies that investigated these strategies beyond expert opinion. Twelve studies recommended that prevention strategies should be particularly targeted at rural areas (Table 4). Improved road infrastructure (n=11) and vehicle design (n=9) were the most recommended prevention strategies. Using an empirical Bayes approach, it was determined that the installation of cable barriers significantly reduces the rate of highway fatalities in the province of British Columbia, Canada42. Education was commonly mentioned as a tool for prevention (n=6), and data from the Rural and Remote Road Safety Study supported graduated licencing systems to enhance driver education29. Furthermore, following a rural MVC, it was determined that the provision of the Royal Flying Doctor Service could lessen the odds of fatality so that they are equivalent to those of metropolitan areas43.
Table 4: Prevention strategies for rural road fatality16,19,26,29-53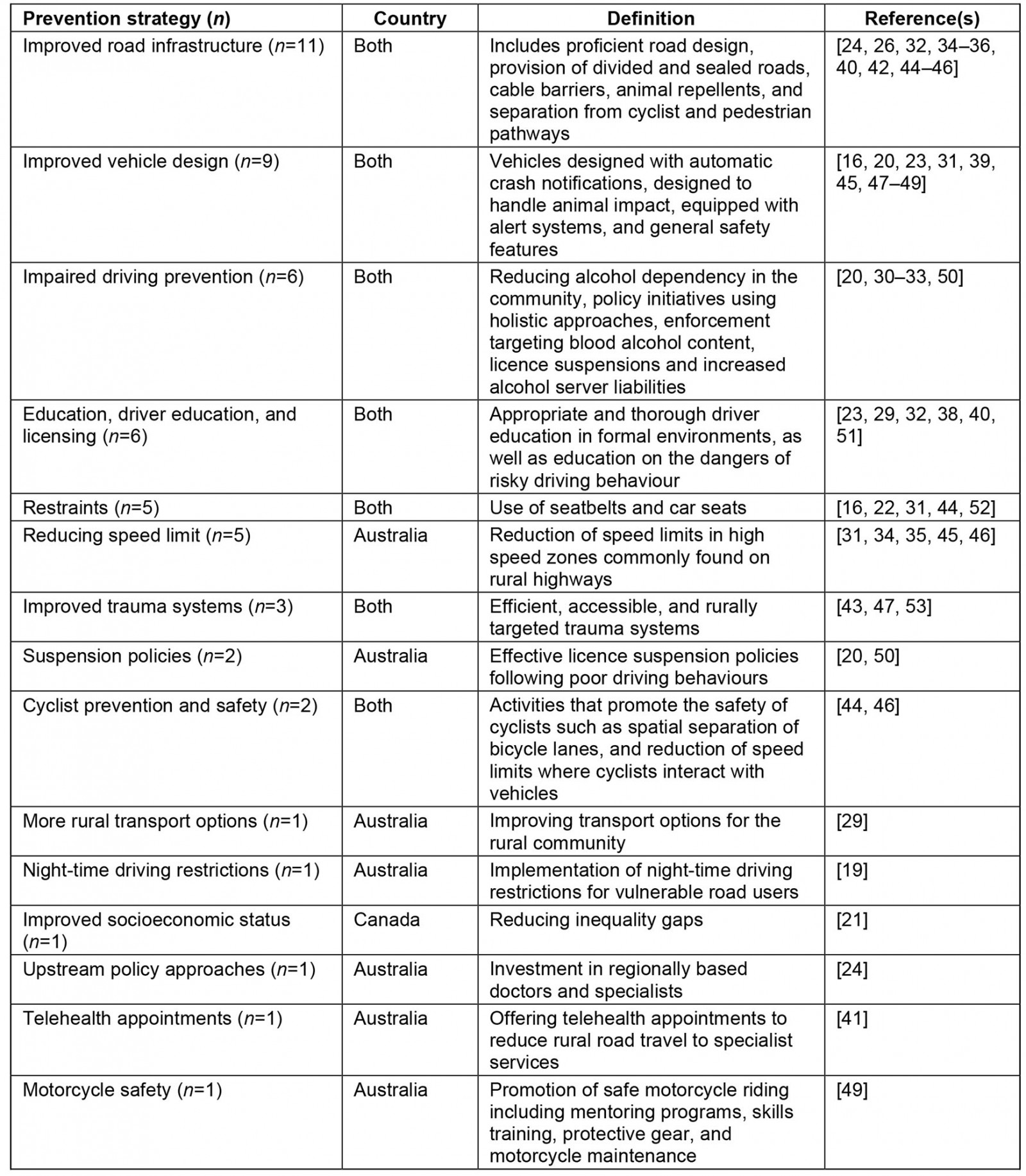
Australia and Canada have many geographical and sociocultural similarities, and as such it is useful to explore epidemiological trends to determine where future prevention efforts should be targeted. In this study, one-third of the articles exploring rurality were from Canada, and the rest were from Australia. Similarities in the rates, risk factors and proposed prevention strategies were found across both countries.
Epidemiology
As expected, the rate of MVC fatalities was higher for rural populations than for urban populations throughout the literature (Table 2). In addition, higher rates were consistent with an increased level of remoteness19. Although high rates do not necessarily indicate a high number of road deaths, this trend suggests Australia and Canada face similar challenges in rural road trauma.
Exploration of risk ratios for age groups was only possible for individuals under 20 years, children aged 0–14 years and young adults aged 17–25 years, but was not determined for other age groups10,16,19. It was common that crude rates were presented for fatal rural MVCs, but there was limited population-based data or no urban comparison. Future studies should provide this information for easier epidemiological calculations.
Risk factors
Due to the large landmasses of Australia and Canada, it was expected that a broad range of contributory factors for rural MVC fatalities would be identified. Although many risk factors contribute to the likelihood of a collision, only factors that were identified for rural fatal crashes were extracted. It is likely that, due to the variable conditions of rural roads, fatal risk factors may differ from those of metropolitan areas. These comparisons were outside of the scope of this study and should be included in further explorations.
Nine common risk factors were defined in the literature, and five were identified in Australia only. The results of this scoping review indicate that the majority of rural MVC fatality risk factors are modifiable. Wundersitz et al suggested that fatal crashes were typically the result of road system failures and not extreme behaviours36. However, the results indicate a need to assess factors on both levels.
A study on risk safety perception demonstrated that drivers perceive rural roads to be less risky than urban roads54. The researchers ascertained that not only the presence of the risk, but also the perception of risk, influences rural road safety. Road safety interventions that reduce exposure to road safety risks have been underutilised55. This is complicated in the context of rural areas, as longer periods of high-speed driving are often required to complete daily activities such as going to school or work9. There is a need for driver education to encompass appraisal of risks and their relevance when considering factors that promote road safety54.
Prevention
Although a wide range of prevention strategies have been shown to reduce road fatalities in metropolitan settings, limited current research exists on their value in rural settings to the best of the author’s knowledge. Only three studies evaluated strategies targeted at rural populations regarding road infrastructure, education and provision of trauma services. The majority of proposed prevention strategies in this study were based on expert opinion and were not evaluated for effectiveness. More work is required to understand the efficacy and proper application of these strategies in rural environments.
Researchers have suggested that the five components of safe road operations (‘five Es’) are engineering, enforcement, education, encouragement and emergency care 56. The prevention strategies identified in this study were mostly consistent with those components, but there was a lack of discussion on encouraging and rewarding positive driving behaviour in both Australia and Canada. Other researchers have recommended a shift from the five Es toward a systems-thinking approach to better accommodate and adapt to human behaviour56. Adopting a systems-thinking approach requires the consideration of the target results and goals of the prevention strategy, the roles of those involved in the system (eg drivers, engineers, policymakers, manufacturers), available resources, the rules of the road system (both formal and informal), and relationships between those in the system (eg individuals, communities and organisations). Further rural road fatality prevention studies should apply this framework to develop a better understanding of the interconnected factors that impact road safety outcomes and safety.
Lower seatbelt compliance rates have been identified in the rural population in comparison to the urban population57. Seatbelt usage was equally identified as a risk factor and as an opportunity for prevention (Table 4)19,28,31,33,37. Descriptive and univariate methods determined that community initiatives in Canada can be effective in sparsely populated regions52. However, this strategy was found to reduce injury rates only, and exploration of seatbelt initiatives and other strategies to reduce rural fatalities are lacking in current literature.
Alcohol
Despite a large focus on alcohol-related MVC interventions, there has been limited improvement over time50. Australia and Canada have similar drinking patterns58,59 and have been identified by the WHO as countries with best-practice laws regarding driving while intoxicated2. However, the results of this review indicated that alcohol and drugs were the most identified risk factors for Australian and Canadian drivers (Table 3). Prevention strategies specific to rural areas ranged from community approaches to licence suspensions (Table 4), although there was limited evidence of the effectiveness of any given strategy in this space. Fatal crashes involving impaired driving in rural and remote settings are a complex issue with many interdependent circumstantial and social factors33. Such social factors may include the venue where consumption takes place (type and location), the nature of the occasion (eg socialising, events, work functions) and drinking partners (eg friends, family, workmates)33. Further work is required to unpack the issues around driving while intoxicated in rural locations to develop targeted strategies, given the small and distributed populations.
Access to health services
The effectiveness of trauma services following a serious MVC is a major determinant of rural fatality rates. Victims of rural MVCs are disadvantaged by the distance between the scene of the accident and major trauma centres48. Rural emergency and ambulance services have been found to spend prolonged time at the scene and experience patient delivery problems53. Trauma care, especially aeromedical retrieval, is a significant secondary prevention strategy60, along with first aid skills61,62 in rural locations. Strategies such as improved access to care and quality of health services were recommended in the research; however, evidence for their effectiveness in the prevention of fatal rural MVCs is lacking in the literature.
Vehicle range
There is a greater diversity of vehicles that use rural roads in comparison to those used on metropolitan roads: from motorcycles to sedans to large agricultural vehicles63-66. This study found that the risk of motorcycle and cyclist fatalities was greater in rural areas than in metropolitan areas29,40. Where vehicle types were compared for rural age groups, little variation was found29. However, there was limited research that compared rural and urban specific groups with vehicle types involved in fatal collisions. Further work should also explore work versus non-work-related incidents, for example the use of quadbikes on roads as opposed to on farms67,68. There is a need for vehicle-specific prevention strategies that help to reduce the overall burden of rural road fatalities.
Climate-related events
Weather events can impact road operations, traffic flow and the roadway itself. Climate change increases the magnitude and frequency of major weather events, presenting a challenge to road safety69. Flooding has been identified as a risk factor in rural Australia and Canada, and while this study found research exploring ‘wet season’ and road fatalities, no articles looked specifically at climate-related issues in rural locations22,70-73. Although snowfall was not found to be a risk factor in this review, it is expected that winter conditions would affect rural road fatalities in Canada, along with freeze–thaw cycles, which are known to deteriorate road infrastructure74. Additionally, comparisons of road safety during wildfire evacuations in both Australia and Canada would be useful, as wildfires threaten many communities in both countries each year, and mutual support has been shared in disaster situations75. Ensuring the safety of people away from population hubs during extreme weather is likely to be a challenge and will potentially require technological solutions.
Limitations
Although fatal crashes were the focus of this review, they do not tell the whole story36. Studies that included rates of serious injury, but not fatal injury, were excluded for the purposes of this article and should be explored further. The lack of prevention strategies specific to rural settings may be an artefact of the search strategy, as studies exploring prevention strategies may not include the term ‘fatality’ or its synonyms. Similarly, significant risk factors in Australia that were not discussed in the included Canadian literature (driver error, stationary objects, animals, risky illegal driving, travelling to obtain health care) may also be a reflection of the search strategy rather than a true reflection of the literature. There may be risk factors that increase the likelihood of a crash and, subsequently, increase the likelihood of fatality. However, unless identified in the literature as road fatality risks, these were excluded. Although some studies included information regarding MVCs and rural populations, we were unable to extract data for MVCs by rurality and, as such, these were not included in this review. Furthermore, conference proceedings, grey literature (including technical reports) and non-peer reviewed sources were excluded, which may have contained relevant epidemiologic, risk factor and prevention data. Studies that were not published in English were also not included, which may have resulted in language bias.
The exploration of Australian and Canadian rural MVC fatality rates is challenged by differencing definitions of rurality. These differences should be considered when making epidemiological comparisons. Additionally, in an attempt to obtain current information on epidemiology, risk factors and prevention, studies that did not fall within the time frame of 2000–2019 were excluded. It is possible that studies dated prior to 2000 may have included information that is still relevant to date.
Conclusion
Rural MVC fatalities present a complex public health challenge. International road safety goals for 2020 established by the WHO were not achieved, indicating that revised strategies are necessary. Addressing rural road fatalities will be required to help meet new 2030 goals in Australia and Canada, which will require targeted action.
An evidence-based systems approach will be required to address the higher rural road rates, including targeting of intoxicated driving, speeding and hazardous road conditions. Evidence-based prevention strategies targeting rural environments are needed. Australia and Canada must invest in strategies that reduce road fatalities in order to achieve goals in road safety and, most importantly, to save lives.




