Introduction
Snakebite was recognised as a neglected tropical disease by the WHO in 2017. Subsequently, in 2019, the WHO released a global strategy to decrease its burden to 50% by 20301. The extensive spread of COVID-19 meant action to address the pandemic (diversion of health system resources, mobility restrictions and economic impacts) took precedence over action on other health conditions, including the effects of snakebite2. To the best of our knowledge, currently there is no quantitative estimation on the effect of containment measures for COVID-19 on snakebite care. Understanding the effect is important for public health agencies, health service providers, as well as policy-makers, to plan for future health systems resilience. We, thus aimed to fill this gap by trying to understand the association between access to snakebite care in India with a health facility being within a COVID-19 cluster-containment zone.
The cluster-containment strategy to prevent spread of COVID-19 was operationalised in India from May 2020. Broadly, the strategy consisted of setting up a perimeter with restricted movement (together with enhanced surveillance and contact tracing), called a containment area, in a defined geographic area with a cluster of COVID-19 cases, based on risk assessment3. The strategy was largely successful in containing COVID-19 in the first wave of COVID-19 in India, but concerns about the strategy not being able to safeguard other acute medical emergencies has been raised.
Methods
We collected data prospectively on hospital admission due to snakebite, referral and modality of transport used to reach the health facility. Data was collected from seven health facilities, in the states of Assam (one community health centre), Bihar (one rural general practice), Maharashtra (one nursing home and one rural general practice), Rajasthan (one tertiary care centre) and Karnataka (one tertiary care hospital and one non-profit primary health centre). We used facility-level data, and treating physicians made decisions on whether snakebites were envenoming or non-envenoming, as per facility protocols. Data were entered every two weeks using a secure online platform (https://redcap.thegeorgeinstitute.org) from May 2020 to October 2020. In addition to facility data, we collected information on whether a health facility was located within a government-declared COVID-19 containment zone or not.
To analyse the effect of a health facility being in cluster-containment zone, we used negative binomial regression analysis. Negative binomial regression analysis is based on Poisson-gamma mixture distribution and can be used to predict count-based data. We chose this analysis method because our dependent variables (number of admissions, referrals and types of transport used) consist of only non-negative integer values and the variance of the dependent variables was greater than the mean. A Poisson mixed model also allows for incorporation of both fixed and random effects for count data4. In our study, this allowed us to incorporate differences in the dependent variable between hospitals (random effect) and within hospital (fixed effect), wherein data have been collected at equal repeated time intervals.
Ethics approval
The study was approved by the institutional ethics committee of The George Institute for Global Health (09/2020), All India Institute of Medical Sciences, Jodhpur (2020-21/2032), and Mysore Medical College and Research Institute and Associated Hospitals (dated 12 May 2020). The study was conducted in accordance with National Guidelines for Ethics Committees Reviewing Biomedical & Health Research During Covid-19 Pandemic (April 2020).
Results
There were 451 admissions due to snakebite (179 envenoming, 39.69%; 272 non-envenoming, 60.31%) in the seven health facilities.
For regression, we used data of 352 admissions due to snakebite (127 venomous, 36.08%; 225 non-envenoming, 63.92%) from five participating health facilities. We excluded two health facilities: one that was declared a COVID-19 facility (which led to a surge of cases, making data collection impossible) and one that recorded only one snakebite admission during the entire study period.
We found that health facilities located within a COVID containment zone had statistically significant decreases in total snakebite admissions (36%; incidence rate ratio (IRR)=0.64; 95% confidence interval (CI)=0.43–0.94; standard error (SE)=0.13; p=0.02)) and in envenoming snakebite admissions (57%; IRR=0.43; 95%CI=0.23–0.81; SE=0.14; p=0.01), in comparison to when the health facilities were not within a COVID containment zone. There was no statistically significant difference for a health facility’s location within a COVID containment zone or not for number of non-envenoming snakebite admissions, or due to different modalities of transport used to reach health facilities (Table 1).
Table 1: Association of incidence rate ratios between facility location within a COVID containment zone or not with facility-level snakebite parameters 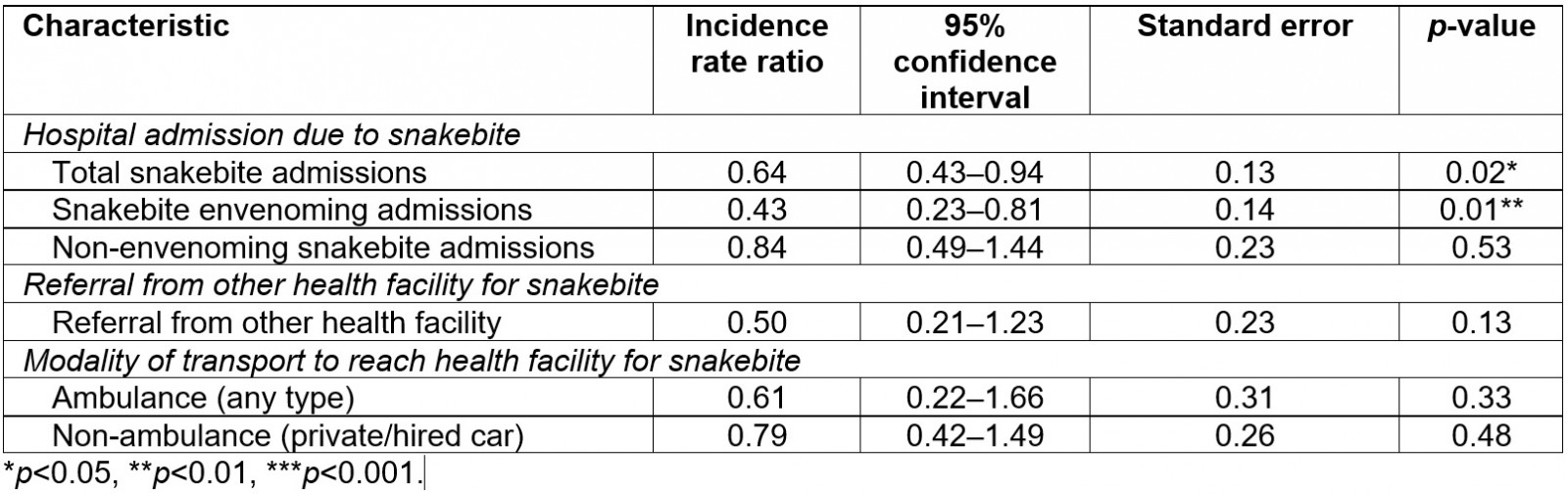
Discussion
The findings of this study suggest a significant decrease in total and envenoming admissions with no difference in non-envenoming admissions or transport modalities due to institution of COVID-19 containment measures in India.
The decrease in total admissions and snakebite envenoming admissions might be due to decrease in community incidence or alteration in care-seeking pathway. The decrease in incidence of snakebite in community is plausible because the change in human activity (less mobility and increased time spent in and around dwellings) due to containment measures might have altered the human–snake-environment interface. It is known that this interface is altered by anthropogenic activity5. It is also possible that the decreased admissions were a result of altered care-seeking pathways.
A qualitative study involving key informants reported perceptions on decreased number of snakebite admissions due to avoidance of a health facility for fear of COVID-19, barriers in testing and several other access issues6. Considering the non-significance for non-envenoming admissions, and the transport modalities to reach health facilities, it is possible that a more complex interaction occurred, consisting of differential alteration of both the human–snake-environment interface and care-seeking pathway between envenoming and non-envenoming cases.
The findings of the present study are context-specific but based on data from a diverse but limited number of health facilities in India. Longitudinal mapping and data collected by transdisciplinary teams on the changing nature of human–snake interactions are needed to understand the issue better. Modelling using data from a wider set of health facilities for several years can provide a better understanding of the effect of COVID-19 on snakebite, including quantitative estimates of the impact across different types of health facilities. Data from India’s national health profile and the Integrated Disease Surveillance Programme might be used for this purpose but it does not report on modalities of transport7 and is mostly limited to public health facilities. It is also known that the official statistics for snakebite cases as captured through these portals is massively undercounted. Research to better understand how care-seeking pathways are altered due to COVID containment measures is also needed.
Conclusion
To the best of our knowledge, this is the only study providing quantitative evidence on the effect of COVID-19 containment measures on access to snakebite care. Understanding the effect of pandemic on snakebite can help develop better multicomponent health systems interventions8 that are resilient to crises such as pandemics and climate change. Augmentation and safeguarding of snakebite care at the primary healthcare system level are necessary when containment measures for pandemic control are being instituted.
Statement of funding
SB is supported by the University International Postgraduate Award by the University of New South Wales. SB has received a NIHR-RSTMH small grant on snakebite.

