Introduction
West Virginia (WV) experiences one of the highest rates of hypertension in the US, and consequently has considerable health and economic burden. Uncontrolled hypertension increases the risk of negative cardiovascular outcomes, including heart attack and stroke, and is a significant contributor to morbidity and mortality worldwide1,2. Those living in rural areas display greater rates of hypertension when compared to the rest of the US, and are disproportionately impacted by community and neighborhood disparities at the healthcare system and individual levels1. Optimal control of hypertension can reduce the risk of both cardiovascular disease and stroke but, despite the widespread availability of treatment to reduce BP, many individuals remain subadequately controlled2,3. Factors including limited access to healthy food and reliable transportation, and distance to clinics, directly impact individuals’ abilities to maintain a healthy lifestyle4-9.
Self-measured blood pressure (SMBP) monitoring is quickly becoming an international standard of care, with a wealth of evidence demonstrating its efficacy in rural communities2,10,11. Cabin Creek Health Systems (CCHS), a federally qualified health center in southern rural WV, implemented SMBP as part of a developing comprehensive program aimed at improving care and outcomes in patients with hypertension and other chronic conditions. As with all healthcare programs, sustainability of care requires the dissemination of data and the collection of resources. With the goal of developing and sustaining a new and improved standard of care, the aim of this work was to perform a mid-point analysis of the SMBP program implemented by CCHS, and its impact on BP control.
Methods
This research represents a mid-point analysis of SMBP implementation at CCHS. Data were retrospectively collected from the electronic health record athenahealth (Athenahealth; https://www.athenahealth.com), by the West Virginia University School of Public Health, Office of Health Services Research. At the time of analysis, six clinic sites in CCHS’s service area were participating in the SMBP program: Cabin Creek, Clendenin, Kanawha City, Riverside, Sissonville, and Sunnyside. The SMBP program, funded by the Health Resources and Services Administration, was initially funded in March 2020, and was funded to February 2023, with a final in-depth evaluation completed in July 2023. Patients qualified for enrollment if they demonstrated current or historical uncontrolled hypertension (systolic ≥140 mmHg and/or diastolic ≥90 mmHg) following a clinical visit with a provider. Once enrolled, patients were equipped with a proprietary iBloodPressure cellular home BP monitoring system, manufactured by Smart Meter (Smart Meter, https://smartmeterrpm.com/solutions). BP values were documented in the integration software TimeDoc Health (TimeDoc, https://timedochealth.com), and athenahealth. For the purposes of this assessment, patient enrollment dates began in January 2021 and ended in November 2022, with evaluation values recorded between August 2021 and June 2022.
Patient data were extracted from athenahealth and analyzed using Microsoft Access. At the time of analysis, 356 patients were enrolled in the SMBP program, but 122 patients were excluded from analyses because they did not have current or historical uncontrolled hypertension at the time of enrollment, or had too few BP values documented to determine pre-enrollment and post-enrollment changes. Patient dropout ranged from 13 to 33 individuals per site, with 21 of 77 individuals excluded from Cabin Creek (27.3%), 25 of 84 individuals excluded from Clendenin (29.8%), 33 of 73 individuals excluded from Kanawha City (45.2%), 13 of 32 individuals excluded from Riverside (40.6%), 30 of 39 individuals excluded from Sissonville (76.9%), and 0 of 9 individuals excluded from Sunnyside (0.0%). Dropout rates were relatively consistent across clinic sites, with the exception of Sissonville and Sunnyside, which exhibited the highest and lowest dropout rates of the six participating clinics.
The average duration of participation in the SMBP intervention was 123 days, with a total of 15 567 remote readings taken and an average of 170 readings per patient (range 10–555). A flowchart detailing the enrollment processes followed, and the criteria used to determine if patients were eligible/ineligible for evaluation are outlined in Figure 1. Pre-enrollment values were calculated as an average of all available systolic and diastolic values taken on the date of enrollment, and post-enrollment values were calculated as an average of all available systolic and diastolic values on the date that readings were last available. Both measures represent each patient’s average blood pressure for a single day. Following exclusions, 33 patients whose BP was controlled at the time of enrollment demonstrated a history of BP fluctuations reaching into the uncontrolled range, indicating the potential for improved BP control. In total, 234 remaining patients were used to assess the SMBP program’s impact on BP control using paired pre-enrollment and post-enrollment BP values. Demographic indices including five or fewer patients were excluded to protect patient confidentiality.
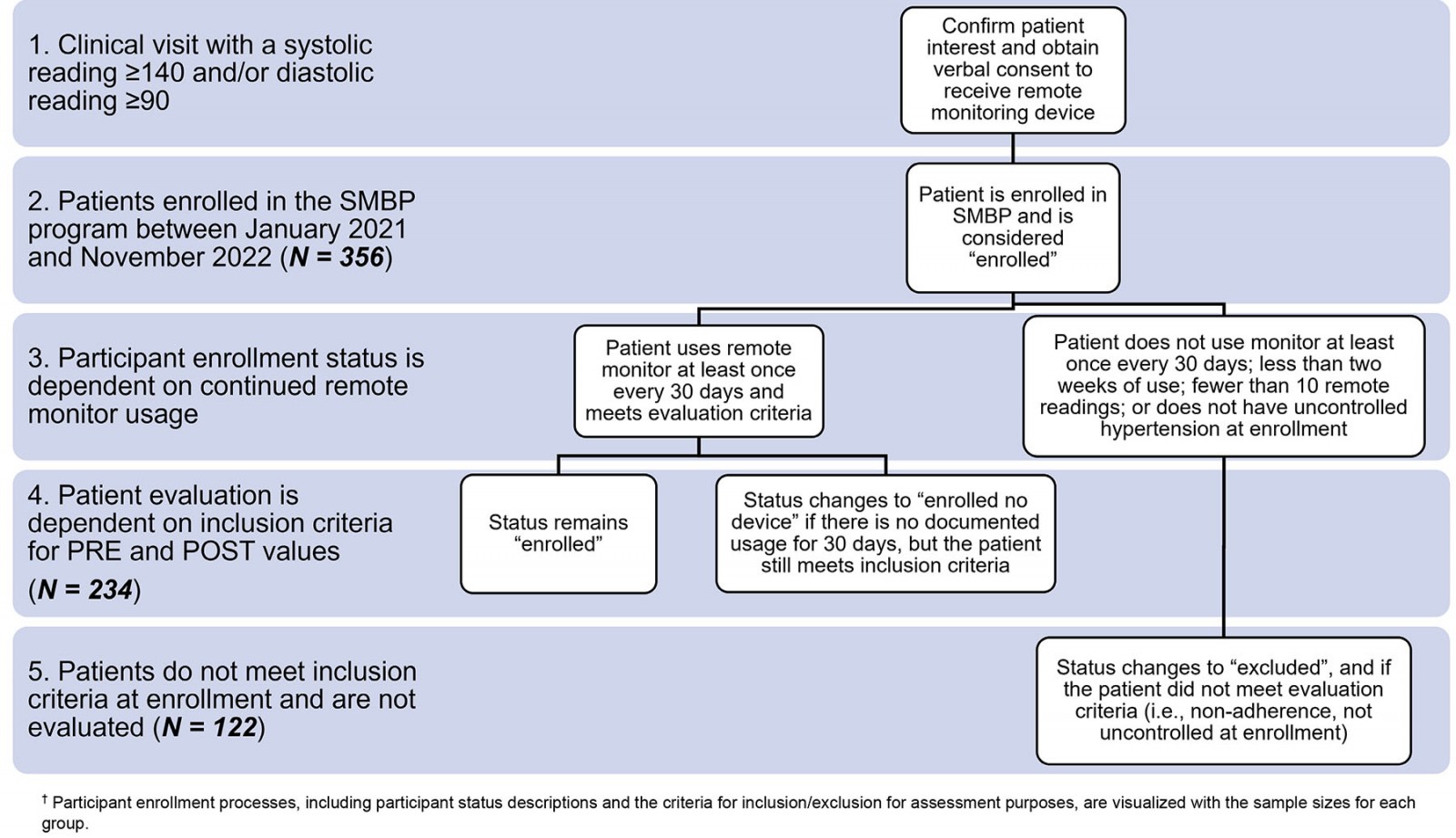 Figure 1: Self-measured blood pressure program and evaluation flowsheet.†
Figure 1: Self-measured blood pressure program and evaluation flowsheet.†
Statistical methods
All statistical methods were performed in Microsoft Excel. Data normality for pre-enrollment and post-enrollment BP readings was assessed using a Jarque–Bera test, which relies on assessments of data skewness (Microsoft Excel function SKEW) and kurtosis (Microsoft Excel function KURT). A Jarque–Bera test was performed using the equation JB=(n/6) * (S2 + (C2/4)) where S and C are values acquired from the skewness and kurtosis tests respectively. Significance was calculated using Microsoft Excel function CHISQ.DIST.RT(JB, 2) to determine normality. Normality assessments for pre-enrollment systolic (p=0.0017), post-enrollment systolic (p≤0.0001), pre-enrollment diastolic (p = 0.9809), and post-enrollment diastolic (p=0.0024) samples indicated that the data overwhelmingly did not follow a normal distribution. Due to its robust nature, a two-tailed, paired, student’s t-test was used to evaluate changes in the average pre-enrollment and post-enrollment systolic and diastolic BP readings. All laboratory results are reported as mg/dL, and data are reported as mean ± standard deviation.
Ethics approval
The retrospective collection of data from patients enrolled in SMBP programming at CCHS was approved by the WVU Institutional Review Board as non-human subjects research (IRB number 2204555632).
Results
Patient demographics are identified in Table 1. Patients were an average age of 57 years, and the majority were female (53.6%). Average laboratory values for triglycerides (187.3±143.9 mg/dL), very low-density lipoprotein (30.9±18.5 mg/dL), and hemoglobin A1c (7.1±2.0%) were higher than the recommended range and were reflective of the International Classification of Diseases (ICD)-10 diagnoses of enrolled patients (Table 1). Of the 234 patients assessed, 219 (93.2%) had a diagnosis of essential (primary) hypertension (Table 1). Optimal laboratory analyte ranges follow the recommendations made by the American Board of Internal Medicine and are provided for reference.
Table 2 uses the American Heart Association BP categorization system to determine the number of patients who meet the criteria for each BP control category. At enrollment, three (1.3%) patients had ‘normal’ BP (systolic <120 mmHg and diastolic <80 mmHg), increasing to six (2.6%) at follow-up (Table 2). Another seven (3.0%) patients had ‘elevated’ BP (systolic 120–129 mmHg and diastolic >80 mmHg) at enrollment, increasing to 16 (6.8%) (Table 2). The number of patients with stage 2 hypertension (systolic ≥140 mmHg and/or diastolic ≥90 mmHg) decreased from 201 (85.9%) to 98 (41.9%), with subsequent increases in patients with stage 1 hypertension (systolic 130–139 mmHg and diastolic 80–89 mmHg), from 81 (34.6%) to 147 (62.8%) (Table 2). Lastly, 26 (11.1%) patients were in hypertensive crisis (systolic ≥180 mmHg and/or diastolic ≥120 mmHg) at the time of enrollment, while none remained in hypertensive crisis at follow-up (Table 2). Percentages do not sum to 100%, as some patients meet the criteria for multiple categories. For example, those with hypertension crisis (systolic ≥180 mmHg and/or ≥120 mmHg) also met the criteria for stage 2 hypertension (systolic ≥140 mmHg or diastolic ≥90 mmHg). Further, both the average systolic and average diastolic BP values decreased significantly. The average systolic blood pressure decreased from 154 mmHg to 138 mmHg, a 16-point decrease (p<0.0001), while the average diastolic blood pressure decreased from 91 mmHg to 84 mmHg, a seven-point decrease (p<0.0001).
In Table 3, patients are in four categories indicating BP control, with BP control assessed within specific demographic indices: ‘met’ (systolic <140 mmHg and diastolic <90 mmHg), ‘systolic not met’ (systolic ≥140 mmHg and diastolic <90 mmHg), ‘diastolic not met’ (systolic <140 mmHg and diastolic ≥90 mmHg), and ‘not met’ (systolic ≥140 mmHg and diastolic ≥90 mmHg). At enrollment, 201 (86.0%) patients had uncontrolled hypertension, with 116 (49.6%) having both uncontrolled systolic and diastolic values (systolic ≥140 mmHg and diastolic ≥90 mmHg). At follow-up, the number of patients with uncontrolled hypertension had decreased from 201 to 98 (41.9%), with only 36 (15.4%) patients having both uncontrolled systolic and diastolic values. The number of patients with BP in the controlled range (systolic <140 mmHg and diastolic <90 mmHg) had increased from 33 (14.1%) to 136 (58.1%). Overall, there was a 44.0% increase in the number of patients in the controlled range. We also observed consistent improvements in BP control across all demographic indices including clinic location, three-digit zip code, and patient sex (Table 3).
Table 1: Participant demographics at enrollment (n=234)†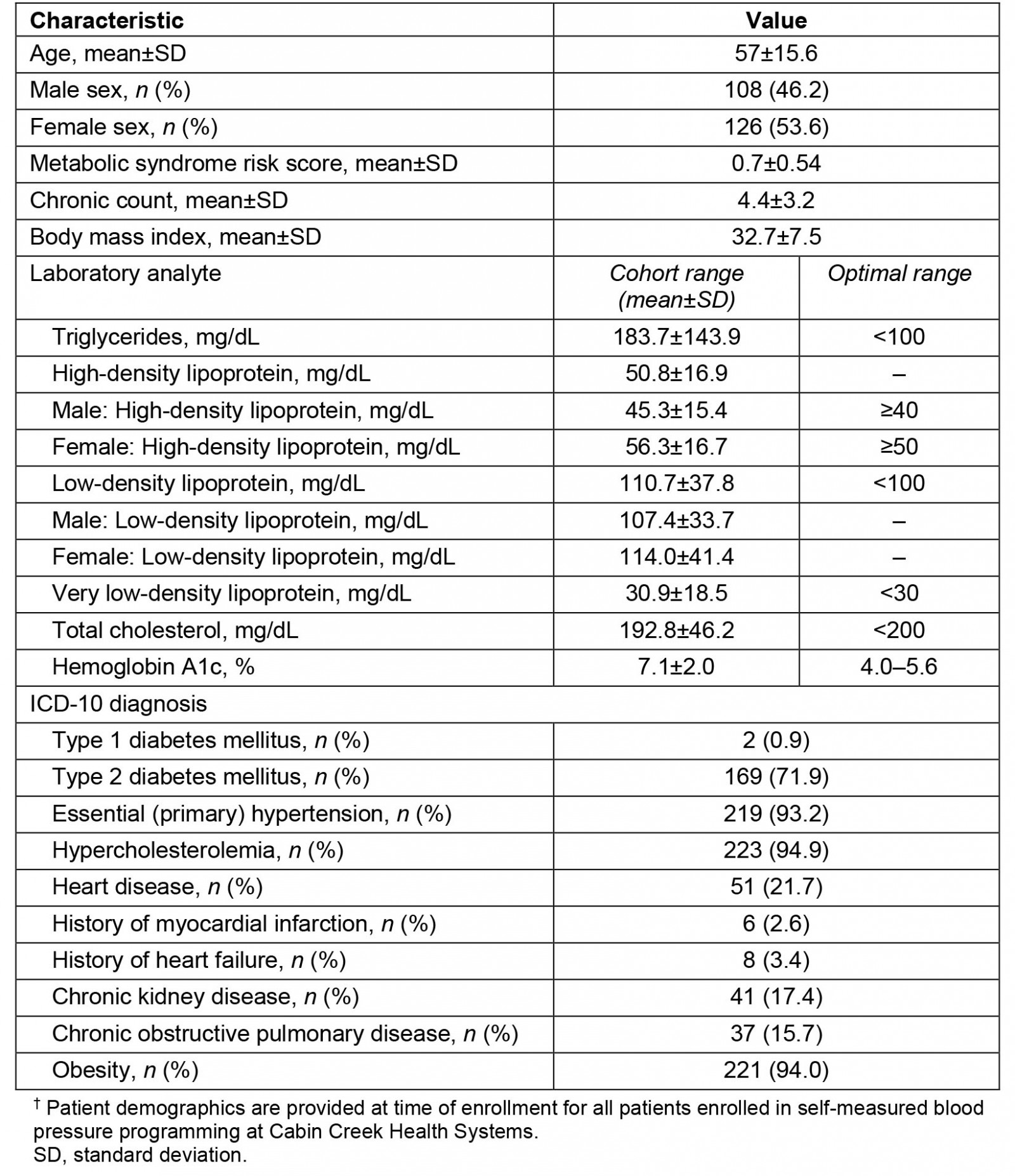
Table 2: Categorization of participant blood pressure (n=234)†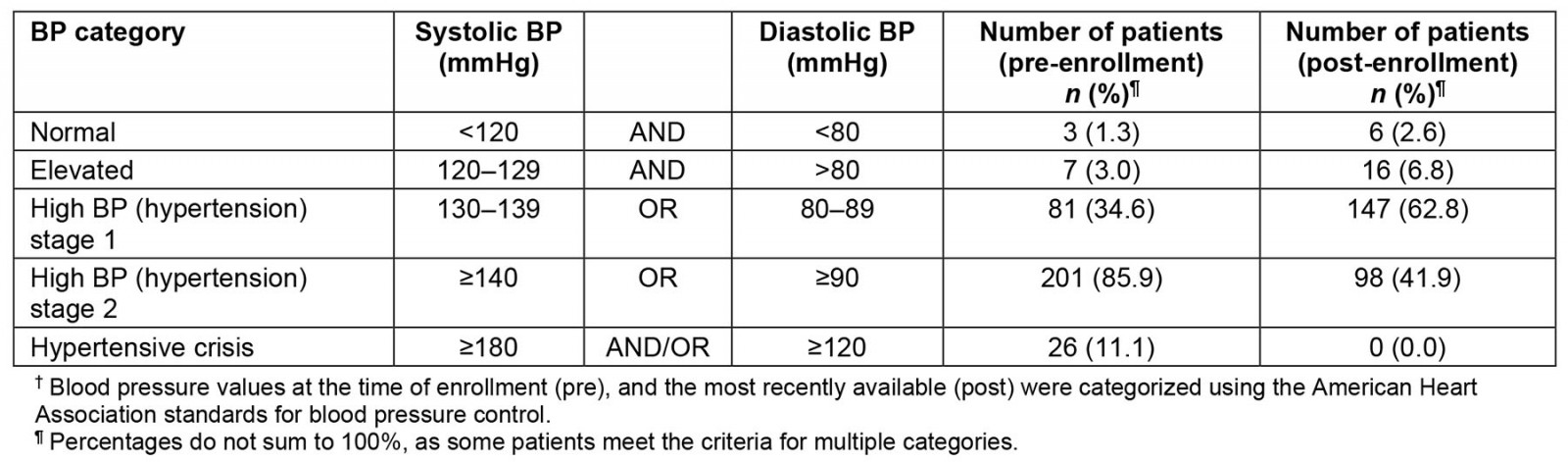
Table 3: Categorization of participant blood pressure by status (controlled or uncontrolled), location, and patient demographics (n=234)†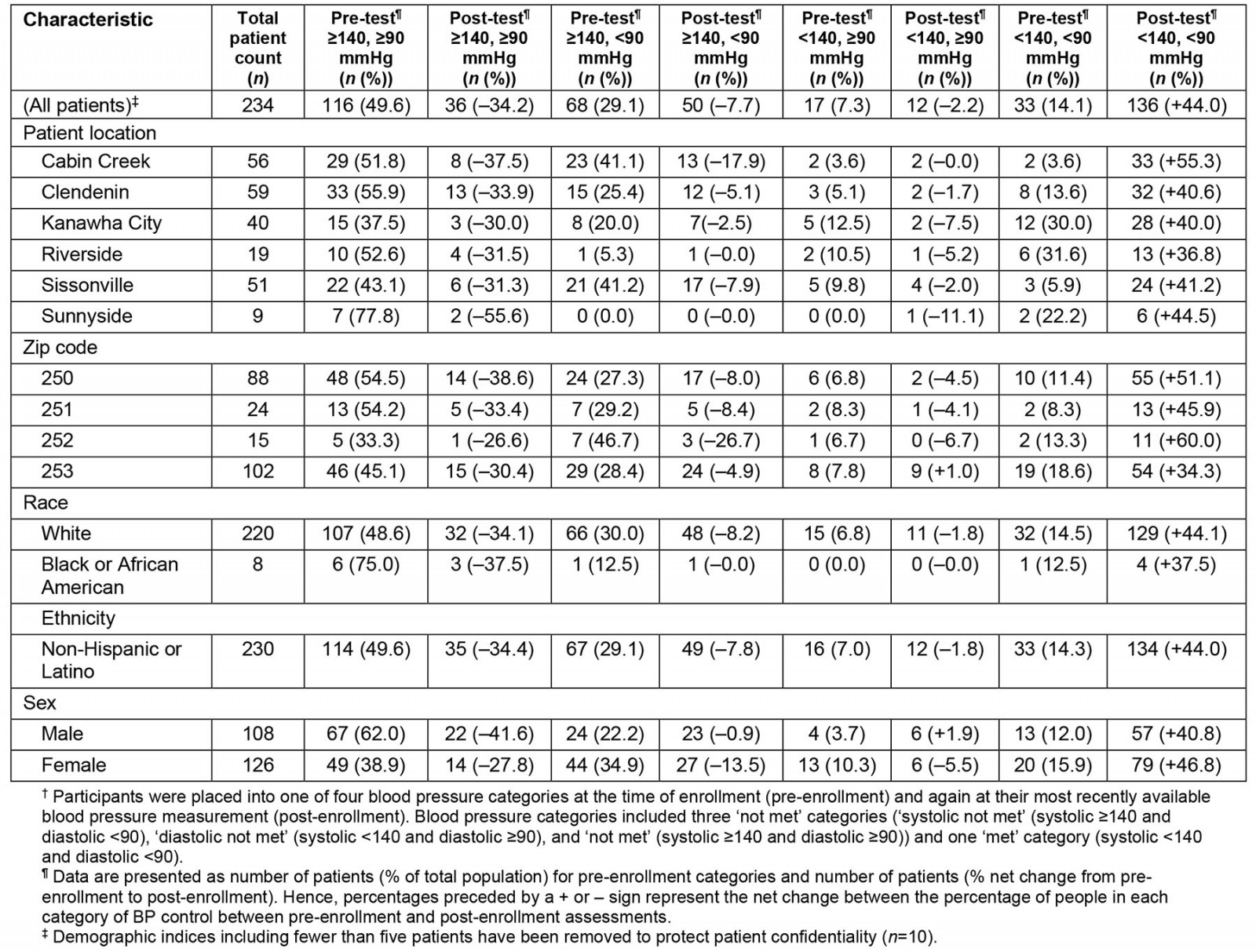
Discussion
The aim of this work was to perform a mid-point analysis of an SMBP program implemented by CCHS, a federally qualified health center in rural southern WV. These data indicate that the implementation of SMBP programming at CCHS contributed to significant improvements in BP control in patients who demonstrated uncontrolled hypertension at the time of enrollment.
The implementation of SMBP programming is largely challenged by the availability of wireless connections for remote data syncing. CCHS’s service area is largely rural, posing issues for the feasibility of remote BP monitoring. More than a third of WV’s population live in rural areas12, and the counties served by CCHS exist within this rural context. Several unique challenges to patient care exist: reduced workforce or staff shortages13,14, lack of reliable transportation6,8, distance to clinics7-9, poor internet access15,16, poor health literacy17, and the stigma of receiving health care18,19. Despite these challenges, each of the six CCHS clinic locations successfully participated in the SMBP program. This widespread implementation allowed for improved patient–provider communication and enhanced patient engagement, and shifted the responsibility for care from the provider to a care team (primary care physician, physician medical assistant, SMBP physician lead, SMBP medical assistant lead, and the hypertension care manager). These interactions are paralleled by improvements in BP control, and are noteworthy because SMBP rarely focuses on outcomes in disparate populations, and scant literature is available assessing SMBP in patients with multiple comorbidities1,20. These data support the use of SMBP programming in improving BP control in these populations.
In addition to these successes, a few challenges and limitations exist. Of the individuals excluded due to non-adherence, the reasons for non-participation remain unknown. Anecdotal reports from providers suggest that rurality and lack of broadband or cellular access are important reasons for inconsistent monitor usage. Also, as a direct result of this mid-point assessment, CCHS improved the SMBP protocol for enrollment and data tracking. First, we identified the need for improved accuracy in data reporting, and data logging issues for criteria such as ‘date of enrollment’ were corrected retrospectively. Second, some patients lacked remote BP readings for extended periods of time (no monitor usage within the previous 30 days), indicating that they had stopped using their remote monitoring device. In response, two new enrollment statuses were introduced. The ‘enrolled no device’ status identifies patients who are enrolled but are unlinked from their remote monitoring device, and the ‘excluded’ status designates patients who were both unenrolled and unlinked from their remote monitoring device. These adjustments improved accuracy of patient counts and documentation of remote monitor usage. The last protocol alteration was the inception of monthly reports containing patients with no remote monitor readings in the previous 30 days, which is regularly distributed to the attributed clinical teams to better track remote monitor usage. Additionally, the SMBP intervention group is being evaluated internally rather than being compared against a control group receiving standard of care. Further evaluation is necessary to determine whether the SMBP system improved BP status more effectively than the standard of care.
Conclusion
We conducted a mid-point assessment of an SMBP program implemented in rural southern WV by CCHS and observed significant improvements in BP control regardless of clinic location, patient demographics, and comorbidities status. These results indicate that this rural health system has been successful in implementing a remote SMBP monitoring program, the findings of which can be informative to other health systems interested in pursuing comparable SMBP efforts. Future directions include the full evaluation of SMBP programming at CCHS and its impact on more specific disparate populations, including focus on race and ethnicity, and comorbidities.
Acknowledgements
We would like to acknowledge the many individuals who have supported and guided the SMBP program at CCHS. Thank you to the CCHS administrators, program coordinators, and staff for guidance in the development and success of this program. Thank you to the WVU Office of Health Services Research team for your expertise in data collection and analysis. Thank you to all the members of the Hypertension Workgroup for making this program a priority. Most importantly, thank you to the physicians and medical assistants who have taken time out of their busy schedules to make this program successful.
Funding
This project was funded by the Health Resources and Services Administration (HRSA) (Award number: 3H80CS00294-18-05).
Conflicts of interest
The authors declare no conflicts of interest.
References
You might also be interested in:
2019 - The Rural Determinants of Health: using Critical Realism as a theoretical framework




